What we do
The Respiratory Infections Section works on diseases caused by, or linked to, viral and bacterial pathogens. The impact of these lung diseases could be greatly decreased if respiratory infection could be prevented. Very little is currently known of what regulate disease severity during respiratory infections. Disorders, such as cystic fibrosis, that make the lung more vulnerable to bacterial sepsis are amongst the commonest human genetic diseases and have a large impact on health and wellbeing.
Despite the enormous impact of lung infections, there is still much to be discovered about the genetic predisposition and the role of the immune response in causing lung disease as well as the optimal way to deliver genetic therapies targeted at the molecular defects.
Our main research aims are:
- understand the role of the immune system in protecting against infection and in causing lung disease
- explore the ways in which disorders such as cystic fibrosis damage the lung’s ability to defend against infection
- develop and test vaccines that might prevent respiratory infection
- understand innate and acquired mucosal responses, developing biomarkers of innate defence and methods by which they may be quantified
- perform human volunteer challenge studies with human pathogens
- test the effects of administration of substances to the respiratory mucosa that act as surrogates for infection, to assist in developing biomarkers of mucosal innate responses
- study the impact of respiratory infections on lung cancer and lung metastasis development
- develop gene therapy-based treatments for a range of lung diseases including CF, alpha 1 anti-trypsin deficiency and pulmonary alveolar proteinosis
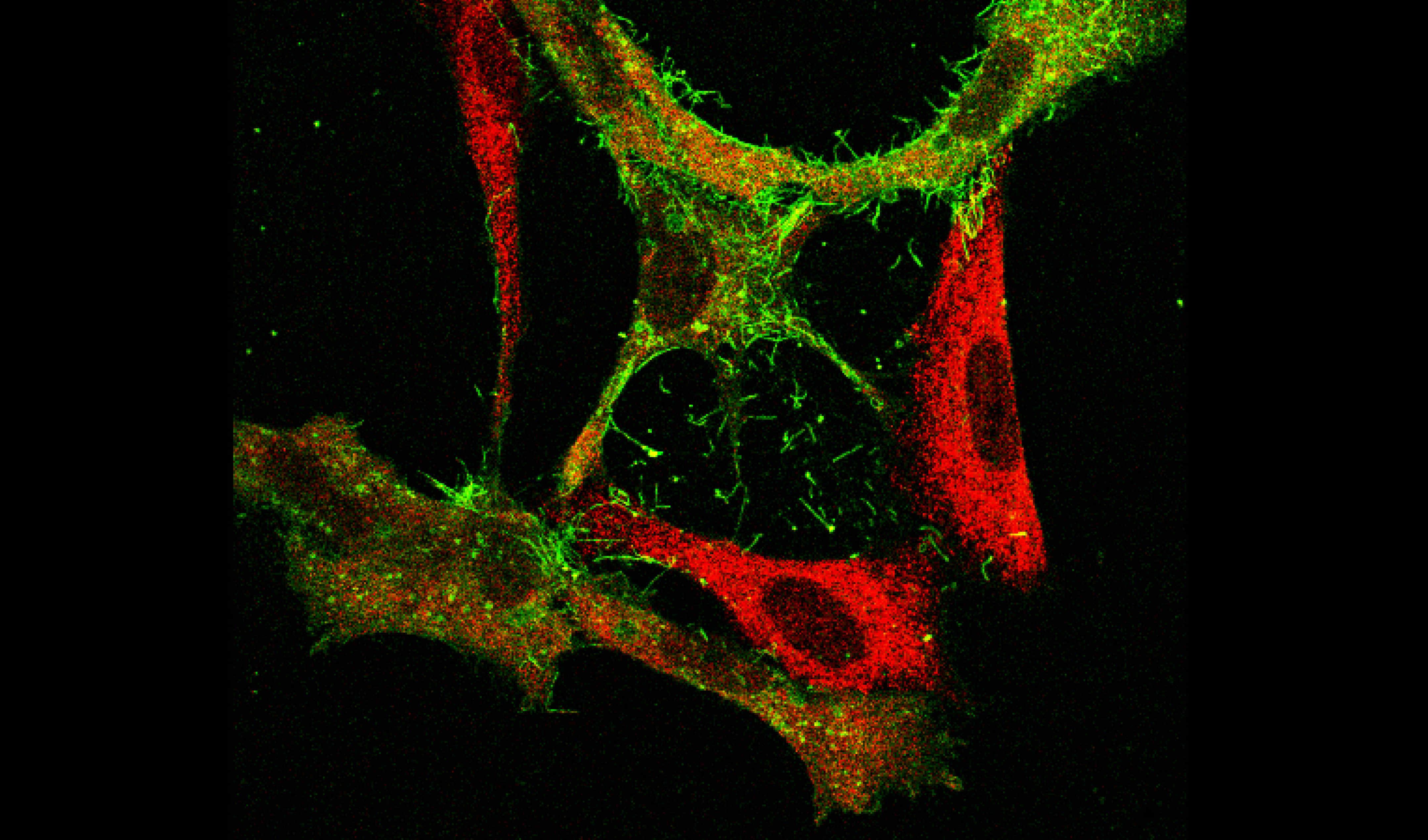
- investigate how bacterial secretion systems or competition systems enable one bacterium to dominate a particular environment
- utilise clinical bacterial strains and samples to better understand lung disease
-
delineate how bacteria sense and respond to their environment or treatment to trigger different bacterial behaviours
Why it is important
Common cold viruses are among the most important human pathogens, causing morbidity and mortality at every stage of life from infancy through to old age. The respiratory mucous membrane extends from the nose down to the lungs, and is extraordinarily well-provided with multi-layered immune defences.
Despite years of study, there is much that remains to be known. The application of modern immunological techniques and concepts provides exciting and rich opportunities to find answers to fundamental questions and problems: what happens in the very earliest stages of viral invasion? How does age affect viral recognition? How does the balance of different immune responses achieve optimal protection, and how can we use this information to make better vaccines? How can the immune system protect without causing immunopathology, and how can we use this knowledge to come up with new treatments?
Cystic fibrosis (CF) patients suffer from chronic lung infection and inflammation which leads to premature death. The median age of death in the UK is currently 33 years. New treatments that improve survival and decrease the significant treatment burden are, therefore, urgently required.
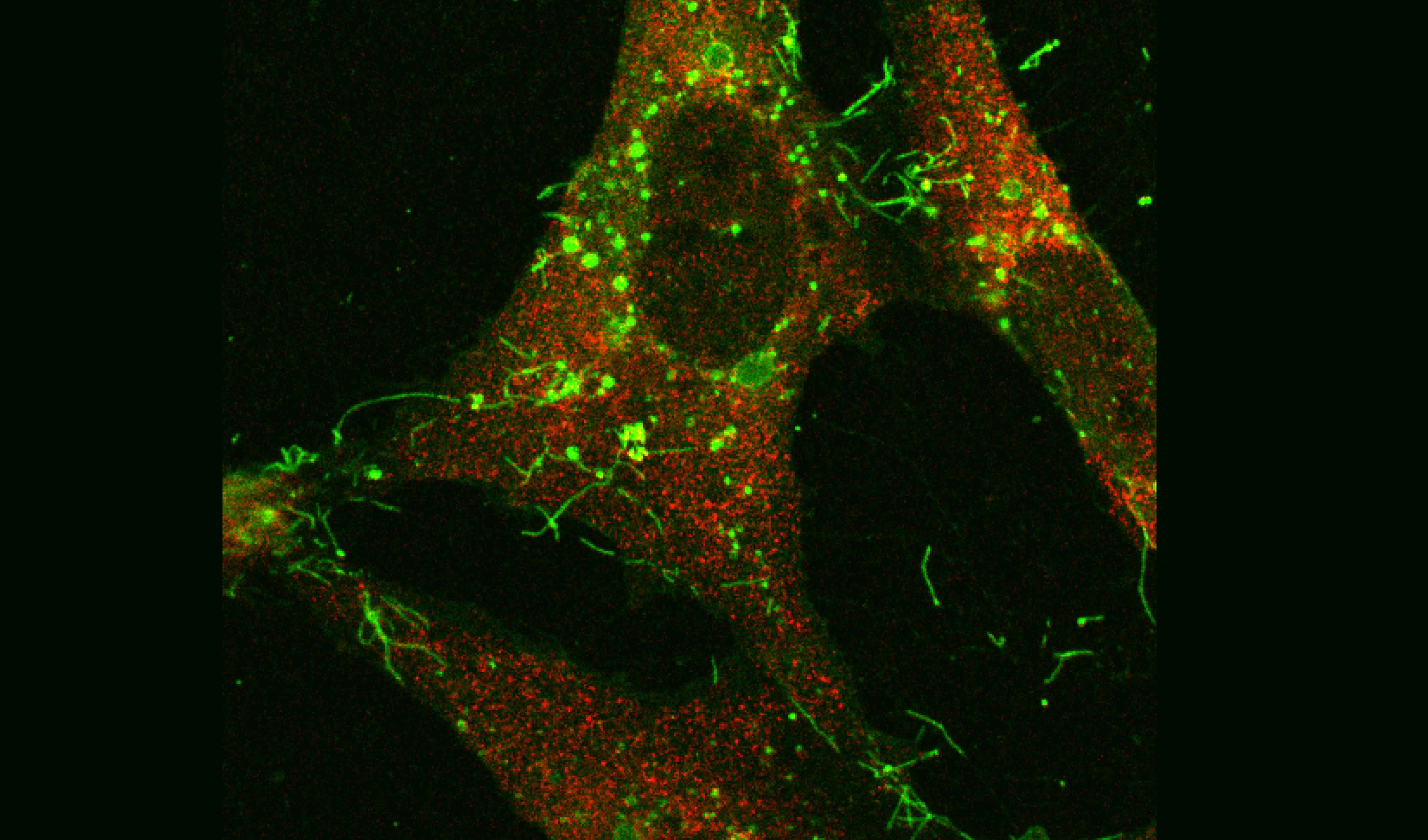
Bacterial Infections contribute greatly to the burden of human and animal disease. Resistance mechanisms to antibiotics are increasing. Better understanding of the mechanism’s that bacteria use to resist treatments or the factors they use to manipulate host cells or kill competing microbes could lead to new ways to combat them. We address these questions using multi-disciplinary approaches including molecular microbiology, structural biology genetics, biochemistry and bioinformatics.
Impact of our research
Our studies have helped to change the way in which the respiratory immune system is viewed. Instead of just being part of the defensive system, the immune system contributes to inflammation and disease in some situations. Our work has helped accelerate vaccine development (e.g. through human infection challenge studies on RSV and influenza), but also provided insights into the mechanisms of airway inflammation caused by infection in conditions such as cystic fibrosis. Our studies on live attenuated influenza vaccine (LAIV) have also demonstrated the vital importance of mucosal antibody and T-cells in providing broader defence against respiratory viruses, extending possibly beyond protection against influenza viruses.
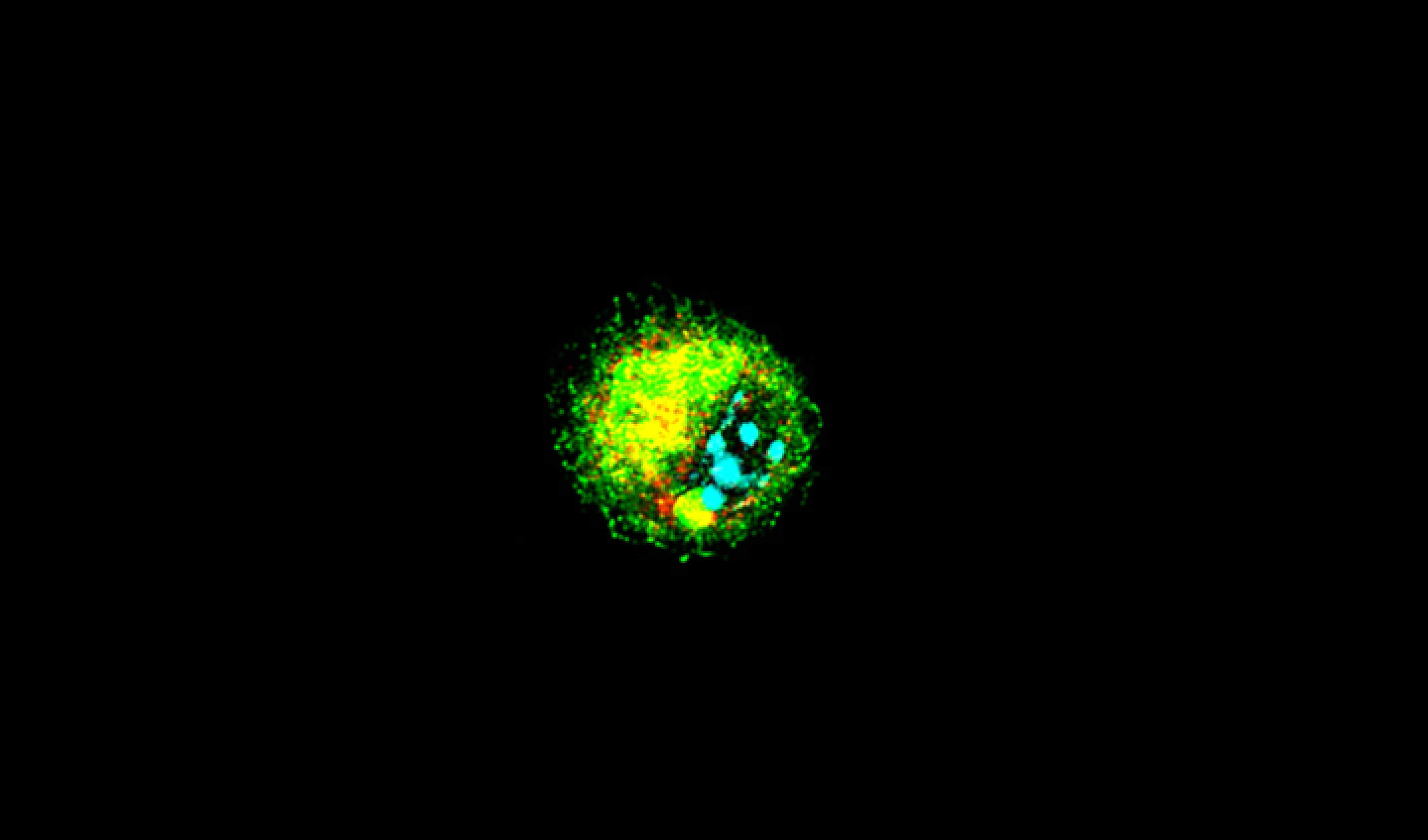
The gene therapy studies have provided the first clinically relevant proof-of-concept that lung function can be ameliorated using this technology in patients with CF. They have also provided a novel platform technology (a pseudotyped lentivirus) which is capable of secreting proteins at therapeutic levels into both the lung and the systemic circulation following delivery to the respiratory tract.
View a selection of publications from the Respiratory Infections Section
Connections
- Strategic Research Centre for Pseudomonas Infection in Cystic Fibrosis - led by Professor Davies
- MRC funded consortium HIC-Vac - co-ordinated by Professor Openshaw
- UK Cystic Fibrosis Gene Therapy Consortium - co-ordinated by Professor Alton the consortium is funded through Wellcome Portfolio and HICF awards and recently completed a tripartite deal with Boehringer Ingelheim and Oxford BioMedica to develop the novel lentiviral platform for cystic fibrosis.
- Imperial component of the EMINENT Consortium - five universities working with GSK on parallel uses of live assets
- The NIHR Imperial Biomedical Research Centre (BRC)
We also run:
- the Imperial College Respiratory Research Unit (ICCRU)
- the St Mary's Flow Cytometry Core Facility - academic lead Dr Fiona Culley
- an animal facility designed specifically for infection research - academic lead Professor Cecilia Johansson
- the NIHR Health Protection Research Unit in Respiratory Infections
- Asthma UK
- BBSRC - GSK
- Cystic Fibrosis Trust
- European Union
- Just Gene Therapy
- Medical Research Council
- MRC/NIHR Efficacy and Mechanism Evaluation Programme
- MRC-Developmental Pathway Funding Scheme
- NIHR Imperial Biomedical Research Centre (BRC)
- National Institute for Health Research
- Rosetrees Trust
- Wellcome
- LifeArc
- The Academy of Medical Sciences
We are very active in public outreach, for example:
- Professor Cecilia Johansson is co-ordinating the Imperial CREST Academy to support scientific mentoring of high school students undertaking British Science Association CREST Awards.
- Professor Peter Openshaw on Science Inspired Tales
Pandemic: Does the Global Media spread Information or Panic
BIOVISION 2015 - Peter Openshaw, "Models for Customized Approaches"
BIOVISION 2015 - Peter Openshaw, "Models for Customized Approaches"
For further information on topics covered in our research please visit theses websites:
Our researchers
Professor Eric W FW Alton FMedSci
Professor Eric W FW Alton FMedSci
Chair in Gene Therapy
Dr Fiona J Culley
Dr Fiona J Culley
Senior Lecturer
Professor Jane C Davies
Professor Jane C Davies
Professor of Paediatric Respirology & Experimental Medicine
Professor Uta Griesenbach
Professor Uta Griesenbach
Professor of Molecular Medicine
Mrs Julia Grizenkova
Mrs Julia Grizenkova
Laboratory Manager
Professor Trevor T Hansel
Professor Trevor T Hansel
Emeritus Professor of Respiratory Pharmacology
Professor Cecilia Johansson
Professor Cecilia Johansson
Professor of Mucosal Immunology
Professor Anne O'Garra
Professor Anne O'Garra
Chair in Infection Immunology
Professor Peter J M Openshaw CBE FMedSci
Professor Peter J M Openshaw CBE FMedSci
Proconsul, Professor of Experimental Medicine
Dr Ryan S Thwaites
Dr Ryan S Thwaites
Lecturer in Respiratory Immunology