Inform
To make a meaningful impact and meet the needs of citizens, policies and practices in healthcare should be informed by the best evidence. That’s why we’re dedicated to using evidence to shape global health policy in areas in need of transformation.
Our work in this sphere is spearheaded by our Centre for Health Policy, which exists to develop, implement and distribute innovative, evidence-based health policies around the world.
Find out how our Institute is uniting world-leading experts and policy-makers to tackle real-world health problems; promoting learning and support; and generating and sharing evidence-based knowledge on a range of pressing health issues.
Highlights from our health policy work
Global State of Patient Safety
Keeping patients safe from avoidable harm should be central to all health systems, and urgent action is needed, leading global health experts warn in the report “Global State of Patient Safety 2023”.
The report provides valuable insight into the current state of patient safety around the world, through analysis of publicly available data from the last two decades.
Produced by the Institute of Global Health Innovation at Imperial College London, and commissioned by the charity Patient Safety Watch, the report includes for the first time a user-friendly interactive data dashboard, case studies of patient safety excellence and a ranking of patient safety in OECD countries.
Without global cooperation, the lack of data in global patient safety could lead to delayed or insufficient action, risking preventable harm and costing lives. The authors urge for data to better reflect the care journeys, perceptions, and experiences of patients.
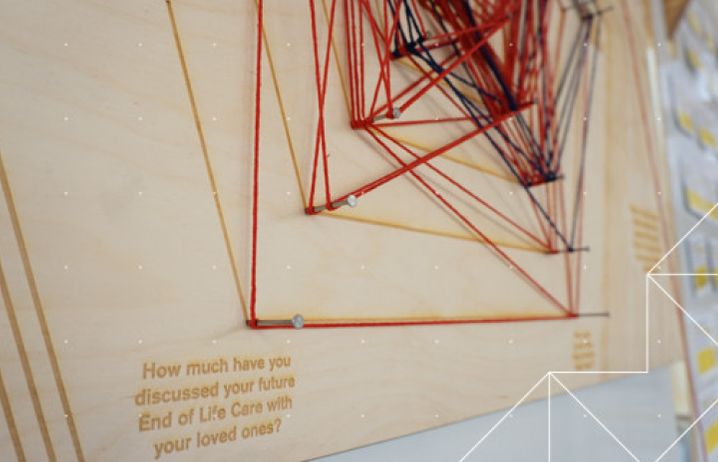
Improving resource allocation for end-of-life care
Research has shown that many patients near the end of life receive high-intensity services without clear evidence of benefits and often at odds with their preferences, with the overwhelming majority of people wishing to remain at home. Yet costly hospital-based care could be avoided if patients were offered high-quality care alternatives outside hospitals.
In partnership with the University of Edinburgh, the University of Lausanne and the Institute for Public Policy Research and public partners, we’re looking at ways to improve the efficiency of health and social care provision at the end of life, and the implications for patients and health systems. We want to find out whether greater efficiency in care resource allocation could enable access to higher-quality and more personalised care for patients.
Our ongoing study is exploring how carers and their loved ones make decisions about end-of-life care, which is necessary to effectively support carers and patients at the end of life to ensure there is high-quality care for all.

Unlocking the benefits of NHS data
The NHS owns long-term health data for the majority of the UK population and this unique asset is poised to be transformative for health, scientific and economic benefit.
Our White Paper, ‘NHS data: Maximising its impact on the health and wealth of the United Kingdom’, offers a framework to guide the proper use of the UK’s health data assets and unlocking their vast potential. Our recommendations include:
- Engaging patients and the public in open and transparent discussions on how their health data is used.
- Establishing clear rules for data access by research organisations and the private sector.
- Recruiting and funding talented data scientists and engineers.
- Establishing government-funded initiatives to improve data quality.
By following these recommendations, policy-makers can harness the potential of the NHS dataset which could drive forward dramatic improvements in health and care, accelerate the development of treatments and technologies, and generate vast income for the UK economy.



