By Andrew Porter
In a paper published in Rheumatology, we carried out a retrospective study of a series of patients with Takayasu arteritis, a systemic vasculitis classically affecting the aorta and its major branches, who developed symptoms of cerebral ischaemia including visual disturbance, dizziness on standing, unilateral hemiparesis, dysphasia and sudden loss of consciousness. Vascular imaging with MR and CT angiography demonstrated extensive arterial stenoses and occlusion of the supra-aortic vessels involving the common carotid, vertebral and subclavian arteries.
All patients were treated with steroids and conventional synthetic DMARDs. Patients who failed to respond sufficiently (as evidenced by return of clinical symptoms, rising ITAS score and/or arterial disease progression on imaging) received early biologic therapy with tocilizumab or infliximab.
In those who received biologic therapy there was a decrease in blood markers of inflammation (ESR and CRP), decreased disease activity scores (ITAS), a reduction in prednisolone dose and no evidence of arterial progression on serial imaging. A cerebral ischaemia score was developed and this fell significantly following effective treatment, with the majority of patients having complete resolution of their neurological symptoms. Only one patient required high risk surgical intervention.
Thus, early use of biologic therapy in those with supra-aortic Takayasu arteritis with cerebral ischaemia reduced the numbers of patients requiring surgical intervention and improved outcomes. We propose that the marked improvement with biologic therapy is secondary to a reduction in arterial wall inflammation and associated oedema, leading to a small increase in the vessel lumen diameter which, according to Poiseuille’s equation, results in an increase in cerebral blood flow equivalent to the change in radius to the power of 4.
Link to publication: https://pubmed.ncbi.nlm.nih.gov/32348517/
Reference
1. Porter A, Youngstein T, Tombetti E, Mason JC. Biologic therapy in supra-aortic Takayasu arteritis can improve symptoms of cerebral ischaemia without surgical intervention. Rheumatology. 2020;59(Supplement_3):iii28-iii32.
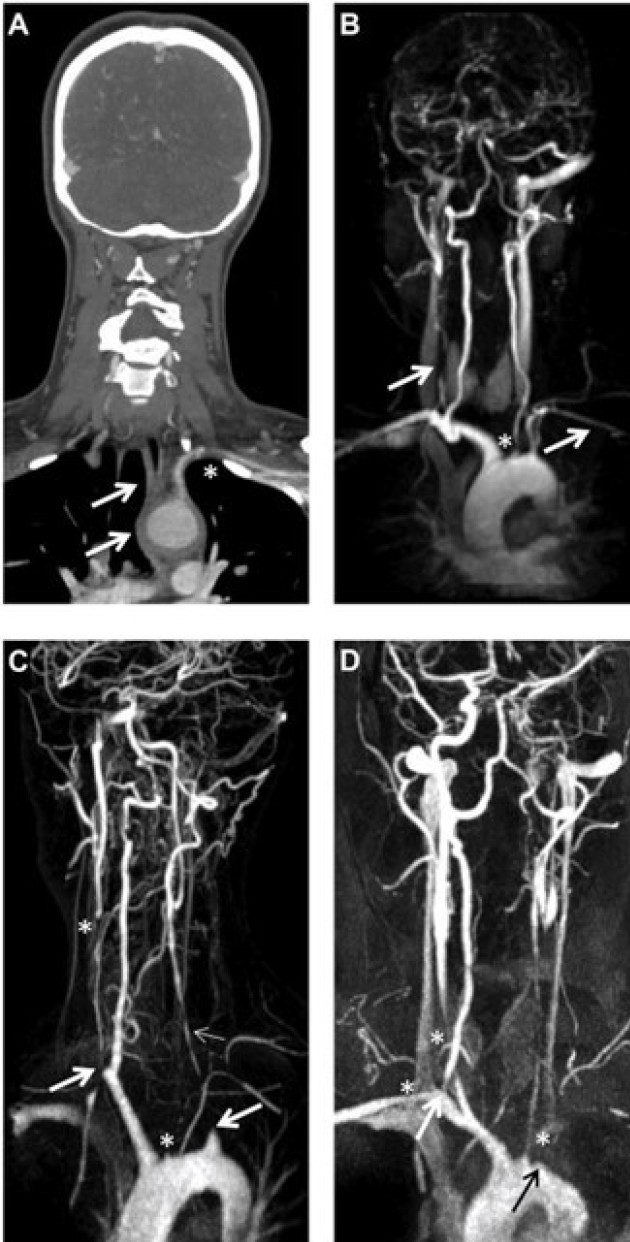
Figure Supra-aortic Takayasu arteritis
(A) CT angiogram of patient 6 demonstrating inflammation affecting the aortic arch that extends to the supra- aortic vessels (brachiocephalic trunk, left CCA and SCA; arrows), with stenosis of the left SCA (star).
(B) MR angiogram of patient 6, with stenosis/occlusion of the right CCA and left SCA (arrows). The star marks the occlusion of the left CCA and proximal narrowing of the left VA.
(C) MR angiogram of patient 3 revealing occluded right and left SCAs (large arrows), occluded CCAs (stars), with an occluded left VA (small arrow) and hypertrophied right VA.
(D) MR angiogram of patient 4 showing occlusion of the left SCA (black arrow), stenosis of the left CCA, right SCA and left VA (stars), with tight proximal stenosis of the right CCA (white arrow). CCA: common carotid artery; MR: magnetic resonance; SCA: subclavian artery; VA: vertebral artery.
General enquiries
For any questions related to the Centre, please contact:
Vasculitis Centre of Excellence Admin
VasculitisCoE@imperial.ac.uk
