Introduction
The Antigen Presentation Research Group (APRG) is located on the Northwick Park and St. Mark's site of the London North West University Healthcare NHS Trust (LNWUH NHS Trust). Directed by Professor Stella C. Knight, the group’s collaboration with clinical colleagues from LNWUH NHS Trust and St Mark’s Hospital and Academic Institute for Colorectal Diseases facilitates world-class studies on human immunology in health and in diseases of the gut and provides higher degree scientific training for clinical and scientific fellows.
Our recent laboratory studies on human immune responses to gut bacteria identifying changes in autoimmunity and cancer, particularly in diseases of the gut, are now impacting on patient treatment. One example, the discovery that vitamin D supplements are essential for Crohn’s disease patients to respond to anti-TNF treatments, and the associated knowledge dissemination, resulted in the requirement to include vitamin D monitoring in St Mark’s Hospital treatment algorithms for Crohn’s patients.
Our research profile also includes participation in two multidisciplinary BBSRC funded research programmes. Firstly as part of the Gut Health and Food Safety (GHFS) Programme of the Institute of Food Research, Norwich, and latterly collaborating on the new Gut Microbes and Health Research programme of the new £multi-million state-of-the-art Quadram Institute at Norwich Research Park, aiming to understand how food and the gut microbiota are linked to the promotion of health and the prevention of disease.
The Antigen Presentation Research Group continues to provide a scientific focus for clinical treatment improvements, building on the scientific knowledge base for human health to inform treatments and combat disease.
Key research interests of our senior team are detailed below.
Our key research
Research themes
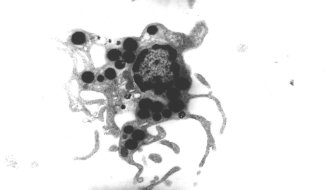
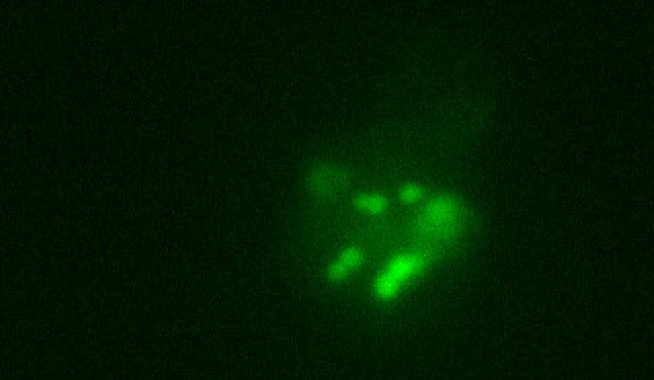
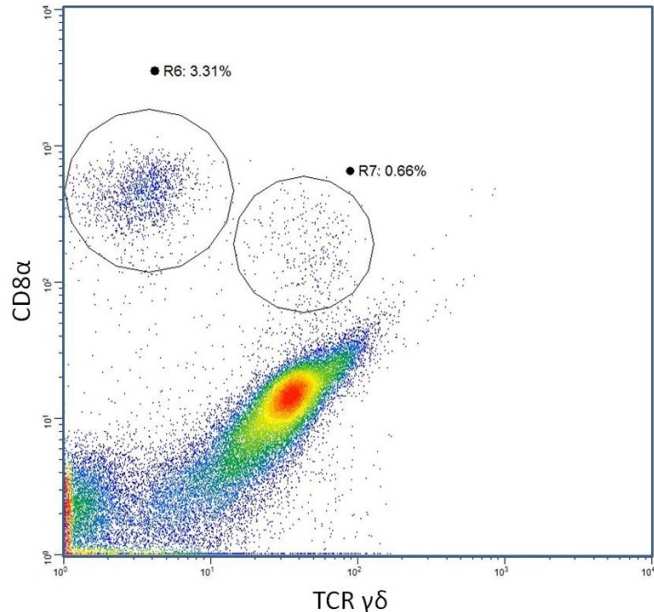
- Human dendritic cell diversity and plasticity - influence of nutrition and microbiota
- Immunity to gut bacteria and Inflammatory Bowel Disease (IBD)
Research group members
Professor Stella Knight
/prod01/channel_3/media/migration/faculty-of-medicine/stella_1625223558582_x4.jpg)
Professor Stella Knight
Senior Research Investigator
Mr Nicholas English
/prod01/channel_3/media/migration/faculty-of-medicine/English,-Nicholas--tojpeg_1469089092101_x4.jpg)
Mr Nicholas English
Honorary Research Associate
Miss Stella Dilke
/prod01/channel_3/media/migration/faculty-of-medicine/dilke_stella_academic_300X300-200X200--tojpeg_1542897405063_x4.jpg)
Miss Stella Dilke
Research Postgraduate
Mr Toby Pring
/prod01/channel_3/media/migration/faculty-of-medicine/pring_toby_academic_300X300-200X200--tojpeg_1542882866721_x4.jpg)
Mr Toby Pring
Research Postgraduate
Dr Sophie Zemenides
/prod01/channel_3/media/migration/faculty-of-medicine/Sophie-profile-pic--t_1509453897365_x1--tojpeg_1542880685982_x4.jpg)
Dr Sophie Zemenides
Research Postgraduate
Funding, Visiting researchers, Collaborators
Funding and acknowledgements
The Antigen Presentation Research Group is grateful for financial support provided by:
- Biotechnology and Biological Sciences Research Council
- London North West Healthcare NHS Trust
- Association for International Cancer Research
- St. Marks Hospital Foundation
- The Broad Foundation
- The Brigid Balfour Memorial Fund
- DSTL (Defense Science and Technology Laboratory)
Collaborators
- Dr Naila Arebi
- Dr Alexandra I F Blakemore
- Prof. Susan K Clark
- Dr Simon M Gabe
- Mr Ian Jenkins
- Mr Georgio Malietzis
- Dr Morgan Moorghen
- Dr Ayesha Akbar
- Dr Lesley Hoyles
Visiting researchers
- Professor Simon Carding
- Dr Ana Carvalho
- Miss Emily Smith
- Dr Diane Williamson
Visiting Students
- Miss Katharine Seton
General enquiries
Antigen Presentation Research Group
North West London Hospitals Campus
Northwick Park & St. Mark's Site
Level 7W, St Mark's Building
Watford Road
Harrow HA1 3UJ
Map directions
Section Manager
Alison Scoggins
a.scoggins@imperial.ac.uk
+44 (0)20 8869 3534