Contact
Prof. Julian R Marchesi
Room 1008, QEQM Building,
St Mary’s Hospital.
+44 (0)20 3312 6197
What we do
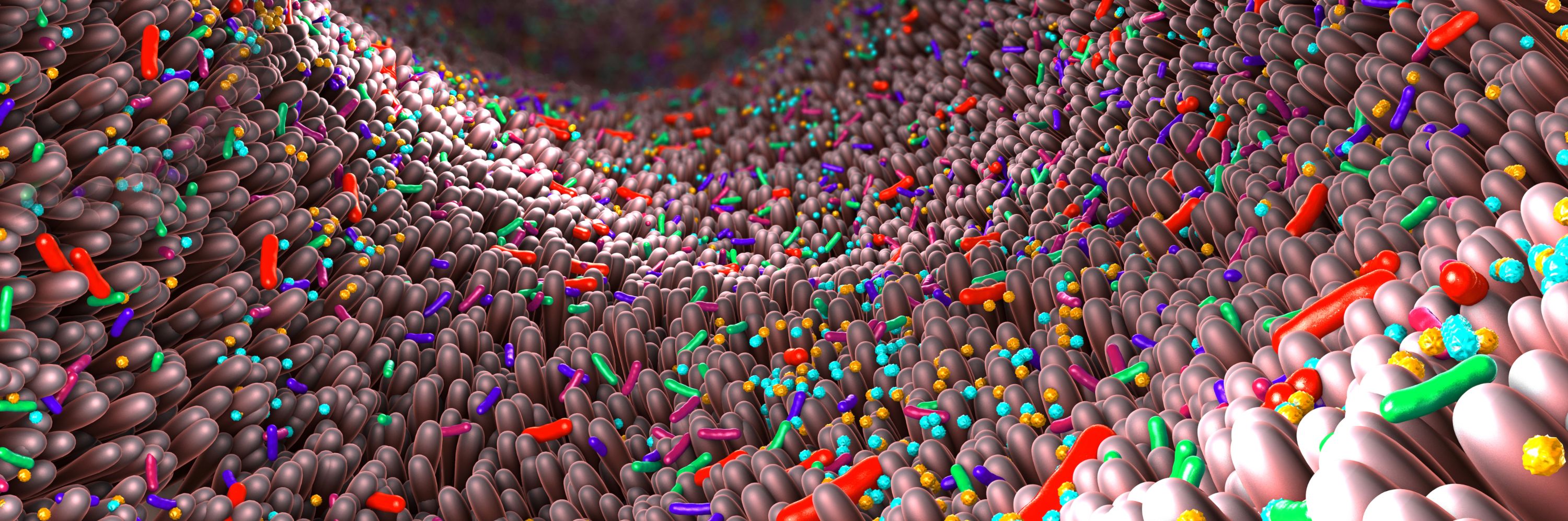
Our group is interested in the role and manipulation of the microbiome of different ecosystems, including the gut and vagina, in health, and how changes in the composition and function of the microbiome characterise and contribute to a range of different disease states. To explore this, we analyse patient samples using a range of advanced systems biology ‘omics’ techniques, including next generation microbial sequencing, metabolomics (done in association with the National Phenome Centre), and proteomics. We then investigate mechanisms as to how these microbiome changes may cause or exacerbate different diseases, using classical microbiology techniques, molecular techniques, or through the use of model systems (including rodent models, or chemostat/ colonic model systems).
Our laboratory includes a close collaboration between scientists and clinicians. One particular significant interest of our group is looking at ways to manipulate the microbiome as a novel paradigm for the treatment of a range of conditions, including via modalities such as probiotics and intestinal (faecal) microbiota transplant (IMT/FMT). A significant area of interest in the group involves using IMT as a discovery tool to better understand host-microbiome interactions, with the aim of understanding mechanisms underlying the efficacy of IMT and exploiting these to produce novel, targeted, microbiome-derived therapeutics.
Why it is important
It is only over the past decade that we have recognised the potential contribution of the microbiome to a range of disease states and therapeutic responses, e.g. stem cell transplants for blood cancers. While we have been able to define distinctive ‘microbiome signatures’ that accompany different diseases, there remains only a relatively small number of scenarios where we have been able to understand specific mechanisms by which the microbiome contributes to the onset and progression of disease, and much more research is required in this field. Furthermore, the concept that manipulating the microbiome may be a therapeutic approach to disease is a surprising new concept that may potentially lead to new therapies and also improve the patient’s therapeutic journey.
How it can benefit patients
A large stream of our work relates to the administration of IMT to patients with a range of different conditions, e.g. infections with antibiotic resistance bacteria to liver disease and cancer treatments. This is obviously directly of benefit to the patients themselves; for instance, a single IMT in a patient with recurrent Clostridioides difficile infection can immediately break the cycle of months of unpleasant symptoms, recurrent antibiotic use and hospitalisation related to colonic inflammation, while an IMT in a patient with blood cancer prior to a stem cell transplant appears to protect them against bloodstream infections and other adverse outcomes after the transplant. However, there are also indirect benefits, as our ability to understand by what mechanisms IMT impacts upon interactions between the microbiome and host will allow us to discover novel, targeted, microbiome-derived therapies.
A further stream of work in the laboratory relates to exploring how the microbiome influences responses to therapies, including: medications that treat inflammatory bowel disease; the degree to which immune checkpoint inhibitor medications successfully treat cancer; or the level of immune response after SARS-CoV-2 vaccinations. In the future, this knowledge might be exploitable for ‘personalised medicine’ approaches, by allowing us to try and better match patients starting treatment to a therapy that we can be confident will work well for them.
Summary of current research
- Characterisation of host-phenome-immune interactions in health and disease through integrative analysis of microbiome, metabonome and other omic datasets.
- Exploring the potential role and mechanisms of efficacy of IMT in a range of clinical settings, including:
- Infective diseases: C. difficile infection, intestinal colonisation with antibiotic-resistant bacteria.
- Metabolic and liver disorders: including obesity, NAFLD, PSC, and cirrhosis.
- Haematological disorders: including blood cancer patients receiving stem cell transplants.
- Rheumatological disorders: including psoriatic arthritis - Understanding how the gut microbiota influences drug responses in a variety of oncological settings and how it can be harnessed to treat drug induced events, e.g. immune checkpoint inhibitor colitis
- Novel approaches to samples and modelling the gut microbiota, for example swallowable capsules that can sample at any site in the GI tract (Nimble Science), using 3D printed swabs for faecal sampling (Opt Industries).
Information
- Funders and related centres
- Useful links for patients
- Collaborators
- Industry
- Publications
- Clinical trials
- Dr Frances Davies, Department of Infectious Diseases, Imperial
- Dr Jiri Pavlů, Dr Andrew Innes: Department of Immunology and Inflammation, Imperial
- Dr Tanya Monaghan, Gastroenterology, Faculty of Medicine, University of Nottingham
- Prof Dina Kao, Division of Gastroenterology, University of Alberta, Canada
- Dr Jessica Allegretti, Gastroenterology, Brigham and Women’s Hospital/ Harvard Medical School, USA
- Prof Tariq Iqbal, Dr Nabil Quraishi, Microbiome Treatment Centre, University of Birmingham
- Dr Christian Lodberg Hvas and Dr Simon Baunwall, Aarhus University, Denmark
- Prof Debbie Shawcross, Dr Simon Goldenberg, Dr Lindsey Edwards, and Dr Blair Merrick, King’s College London/ King’s College Hospital
- Dr Jarosław Biliński, Prof Grzegorz W Basak, Medical University of Warsaw, Poland
- Prof. Johann de Bono, Institute of Cancer Research
- Ghani R, Mullish BH, Davies FJ, Marchesi JR. How to adapt an intestinal microbiota transplantation programme to reduce the risk of invasive multidrug-resistant infection. Clin Microbiol Infect. 2022 Apr;28(4):502-512. doi: 10.1016/j.cmi.2021.11.006. PMID: 34826617. (https://pubmed.ncbi.nlm.nih.gov/34826617/)
- Innes AJ, Mullish BH, Ghani R, Szydlo RM, Apperley JF, Olavarria E, Palanicawandar R, Kanfer EJ, Milojkovic D, McDonald JAK, Brannigan ET, Thursz MR, Williams HRT, Davies FJ, Marchesi JR, Pavlů J. Fecal Microbiota Transplant Mitigates Adverse Outcomes Seen in Patients Colonized With Multidrug-Resistant Organisms Undergoing Allogeneic Hematopoietic Cell Transplantation. Front Cell Infect Microbiol. 2021 Aug 27;11:684659. doi: 10.3389/fcimb.2021.684659. PMID: 34513724; PMCID: PMC8430254. (https://pubmed.ncbi.nlm.nih.gov/34513724/)
- Li JV, Ashrafian H, Sarafian M, Homola D, Rushton L, Barker G, Cabrera PM, Lewis MR, Darzi A, Lin E, Gletsu-Miller NA, Atkin SL, Sathyapalan T, Gooderham NJ, Nicholson JK, Marchesi JR, Athanasiou T, Holmes E. Roux-en-Y gastric bypass-induced bacterial perturbation contributes to altered host-bacterial co-metabolic phenotype. Microbiome. 2021 Jun 14;9(1):139. doi: 10.1186/s40168-021-01086-x. PMID: 34127058; PMCID: PMC8201742. (https://pubmed.ncbi.nlm.nih.gov/34127058/)
- Ghani R, Mullish BH, McDonald JAK, Ghazy A, Williams HRT, Brannigan ET, Mookerjee S, Satta G, Gilchrist M, Duncan N, Corbett R, Innes AJ, Pavlů J, Thursz MR, Davies F, Marchesi JR. Disease Prevention Not Decolonization: A Model for Fecal Microbiota Transplantation in Patients Colonized With Multidrug-resistant Organisms. Clin Infect Dis. 2021 Apr 26;72(8):1444-1447. doi: 10.1093/cid/ciaa948. PMID: 32681643; PMCID: PMC8075030. (https://pubmed.ncbi.nlm.nih.gov/32681643/)
- Mullish BH, McDonald JAK, Pechlivanis A, Allegretti JR, Kao D, Barker GF, Kapila D, Petrof EO, Joyce SA, Gahan CGM, Glegola-Madejska I, Williams HRT, Holmes E, Clarke TB, Thursz MR, Marchesi JR. Microbial bile salt hydrolases mediate the efficacy of faecal microbiota transplant in the treatment of recurrent Clostridioides difficile infection. Gut. 2019 Oct;68(10):1791-1800. doi: 10.1136/gutjnl-2018-317842. Epub 2019 Feb 11. PMID: 30816855; PMCID: PMC6839797. (https://pubmed.ncbi.nlm.nih.gov/30735608/)
- McDonald JAK, Mullish BH, Pechlivanis A, Liu Z, Brignardello J, Kao D, Holmes E, Li JV, Clarke TB, Thursz MR, Marchesi JR. Inhibiting Growth of Clostridioides difficile by Restoring Valerate, Produced by the Intestinal Microbiota. Gastroenterology. 2018 Nov;155(5):1495-1507.e15. doi: 10.1053/j.gastro.2018.07.014. PMID: 30025704; PMCID: PMC6347096. (https://pubmed.ncbi.nlm.nih.gov/30025704/)
Our researchers
Prof Julian Marchesi
/prod01/channel_3/media/images/people-list/Prof-Julian-Marchesi.jpeg)
Prof Julian Marchesi
Professor of Digestive Health
Dr Benjamin Mullish
/prod01/channel_3/media/images/people-list/Dr-Benjamin-Mullish.jpeg)
Dr Benjamin Mullish
NIHR Clinical Lecturer
Dr Despoina Chrysostomou
/prod01/channel_3/media/images/people-list/CHRYSOSTOMA-Despoina-18.02.2025-6.jpg)
Dr Despoina Chrysostomou
Postdoctoral Research Associate
Cansu Sevim
/prod01/channel_3/media/images/people-list/Cansu-Sevim-Profile-Picture.JPG)
Cansu Sevim
Research Postgraduate
Ms Lauren Roberts
/prod01/channel_3/media/images/people-list/laura.jpg)
Ms Lauren Roberts
Research Technician in Microbiology