Contact
Lab/office contact number: 0203 315 3332
3rd Floor, Chelsea and Westminster Hospital, Chelsea and Westminster Campus
What we do
Female reproductive health is a vital yet often overlooked area of medical research. Our work aims to address this historical neglect, contributing to a future where female reproductive health receives the attention it deserves.
The group’s focus is on two questions:
- How do immune cells in the uterus support a healthy pregnancy?
- How do interactions between the immune and female reproductive systems influence health more broadly?
We are exploring the role of innate immune cells in the uterine mucosa in facilitating successful placental implantation, protecting against vertical transmission of infections, and initiating labour.
Additionally, we are investigating how acute inflammation can cause temporary changes in menstrual cycle length and flow, and the bidirection relationship between chronic inflammatory conditions and menstrual cycles.
Why it is important:
Failures in placental implantation can result in various pregnancy complications, including recurrent implantation failure, recurrent pregnancy loss, pre-eclampsia and preterm birth. Similarly, disruptions in the timing of labour can lead to either preterm birth or post-term pregnancy, the latter of which increases the risk of stillbirth. By studying how implantation and labour occur in healthy pregnancies, we can identify cells and molecules that may serve as targets for preventing these complications.
The interactions between the immune system and the female reproductive system also have implications beyond pregnancy. During the COVID-19 pandemic, anecdotal reports suggesting that vaccination affected menstrual cycles contributed to vaccine hesitancy among young women. However, due to a lack of research, we were unable at the time to provide clear explanations about the immune response’s normal effects on menstruation. Conversely, many individuals with long COVID noticed fluctuations in their symptoms based on their menstrual cycles. Investigating these interactions, as well as the relationship between menstrual cycles and other chronic conditions, could reveal new opportunities for using reproductive hormones in disease management.
Summary of current research
The effect of immune responses on the menstrual cycle, led by Abigail Goodship.
Using a mouse model and observational studies of healthy volunteers receiving routine vaccinations, Abigail will define how acute inflammation affect oestrus and menstrual cycles. This project also includes an iCASE component, in collaboration with industry partner Hertility, to examine how chronic inflammatory conditions and autoimmune diseases affect reproductive health.
Uterine NK cell subsets in the control of HCMV, led by Eleanor Bradley.
We have previously shown that tissue-resident NK cells in the liver are uniquely able to control HCMV. This project seeks to determine whether tissue-resident NK cells in the uterus are similar, and define the importance of this for preventing vertical transmission of HCMV.
Defining the role of a novel population of decidual macrophages in the initiation of labour, led by Emilie Paterson.
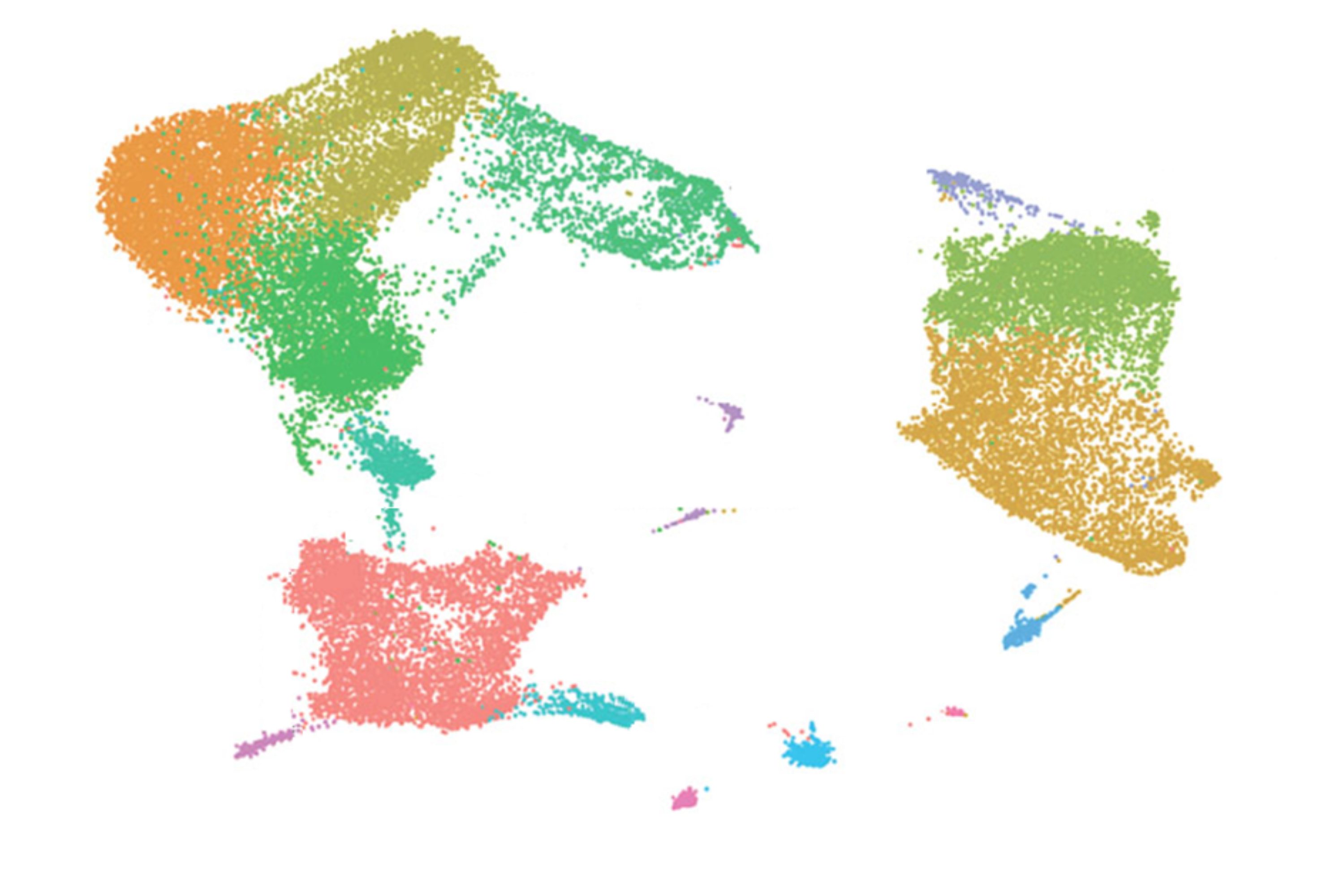
By examining single cell RNA sequencing data, we identified a novel macrophage subpopulation that is more numerous and active during labour, and that produces MMPs that may mediate rupture of membranes. Emilie has designed a flow panel to examine these a range of samples across the spectrum of labour, validating the RNAseq findings and determining whether the changes described precede the initiation of labour.
The role of uterine natural killer cell subsets in mediating placental implantation, led by Shreya Sheth.
Uterine NK cells consist of three subsets and our previous work implicates one of these (uNK1) as most numerous and active at the time of placental implantation. Shreya is examining the activity of these cells in fertility patients, compared to fertile controls attending for contraceptive coil fitting. She is developing a “placenta-on-chip” model to better understand the mechanisms by which uterine NK cells promote placental implantation.
Information
Funders
Industry Partners
Our researchers
Dr Victoria Male
/prod01/channel_3/media/images/people-list/Victoria-Male.JPG)
Dr Victoria Male
Principle Investigator
Dr Shreya Sheth
/prod01/channel_3/media/images/people-list/Shreya-Sheth.jpg)
Dr Shreya Sheth
MRC-funded Clinical Research Fellow
Abigail Goodship
/prod01/channel_3/media/images/people-list/Abigail-Goodship.jpg)
Abigail Goodship
Research Postgraduate
Eleanor Bradley
/prod01/channel_3/media/images/people-list/Ellie-Bradley.jpg)
Eleanor Bradley
Research Postgraduate
Emilie Paterson

Emilie Paterson
Research Assistant