Early life and post-pregnancy interventions to improve maternal and child health
Why is it important
Pregnancy can be thought of as a stress test that identifies a woman’s subsequent disease risks. For example, those with gestational diabetes mellitus (GDM) are more likely to develop type 2 diabetes in later life and those with intrahepatic cholestasis of pregnancy are more likely to develop future liver disease. Furthermore, the children of women with these disorders have an increased risk of adiposity, dyslipidaemia, insulin resistance, liver steatosis and related cardiometabolic risk factors. If we can identify pregnant women (and their children) who are at risk of these future health risks we can aim to target interventions at these groups at an earlier stage to improve their future health.
Summary of current research
Studies of future health of women with ICP
As women with ICP are known to be at increased risk of cardiometabolic disease, we are prospectively reviewing women with previous ICP to establish whether they have subsequently developed liver or biliary tract disease. In parallel we are evaluating the contribution of genetic risk factors in these women.
Research evaluating the impact of maternal metabolic disorders on fetal heart rhythm and risk of stillbirth
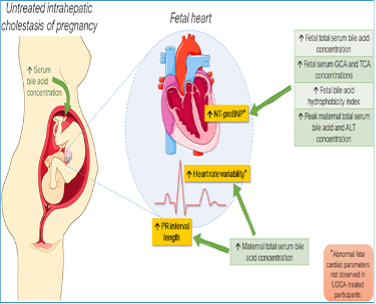
The babies of women with ICP and diabetes have an increased risk of stillbirth, likely related to the effect of the metabolic changes in these conditions affecting the heart of the unborn baby. We are using fetal electrocardiograph (fECG) monitoring to study the impact of ICP and diabetes on the heart rhythm of the baby. We have shown that high bile acid concentrations in the blood of ICP fetuses can cause abnormal heart rhythms and ongoing research is evaluating this phenomenon in more detail in collaboration with Professor Steven Niederer’s team (NHLI). In collaboration with Professor John Simpson (KCL/Evelina Children’s Hospital) we are using fECG to study other causes of abnormal heart rhythm in the fetus. This includes a project to study fetal ECGs in the babies of women with type 1 and type 2 diabetes.

Clinical trials to improve maternal, fetal and child health
The Williamson group is leading and/or facilitating clinical trials of drugs to treat ICP and GDM. Alongside evaluating the impact on maternal disease, the team is also studying the impact of the study drugs on the unborn baby. Current work is focussing on:
- Does the ileal bile acid transport inhibitor maralixibat improve maternal features of ICP?
- Can rifampicin treatment improve maternal itch in ICP, and does it improve other features of the disease for mother or baby?
- What is the impact of ursodeoxycholic acid on maternal glycaemic control in GDM?
- How does metformin (or UDCA) impact maternal gut microbiota and gut signalling to alter glycaemia in GDM?
Interventions to reduce the adverse health impact of childhood obesity
As the children of women with GDM and ICP have increased risk of adiposity and steatosis, and also given the rising rates of childhood obesity, we are aiming to design non-pharmacological interventions that improve the metabolic health of children and young people. Using a combination of murine models and human studies we are evaluating the impact of intermittent cold exposure on brown adipose tissue function, serum lipids and liver steatosis.
- Mouse studies are comparing the impact of intermittent cold exposure on brown adipose tissue (BAT), white adipose tissue (WAT), liver phenotypes, serum lipids and other markers of metabolic health in mice fed a normal chow diet or a high fat diet.
- In parallel we are evaluating the impact of neonatal cold exposure on BAT/WAT function and metabolic health in the offspring of dams fed a high fat diet (to mimick gestational diabetes) or a normal diet.
- Human studies are evaluating the impact of intermittent cold exposure using a wearable ‘cooling jacket’ in young people with liver steatosis and control individuals of normal weight.

How the research benefits patients
If we identify effective interventions to improve the future health of women with maternal metabolic diseases and/or their children this will have an important impact on management of families after experiencing complicated pregnancies.
Researchers
- Sian Chivers (based at St Thomas’ Hospital)
- Alice Mitchell
- Madeleine Reid
- Aleck Jones
- Luiza Manna
- Caroline Ovadia
- Catherine Williamson