New nanotech weapons could reduce deaths from bacterial infections
by Sam Wong
Professor Sunil Shaunak's research uses new tools from nanotechnology to manipulate the immune system
The thrill of discovery came early in Sunil Shaunak's medical career. While at Duke University in the mid-1980s he remembers looking down a microscope and seeing the virus that eventually explained the AIDS epidemic. Now, after 27 years of treating and researching infectious diseases at the Royal Postgraduate Medical School and then in the Department of Medicine at Imperial, he reflects on a career that has seen AIDS change from a deadly disease to one whose treatment is as routine as that of diabetes.
But infections still take a huge toll on human lives. "Even though doctors have a powerful arsenal of antibiotics, antivirals and antifungals at their disposal, patients are still dying," Professor Shaunak says. The reason, he asserts, is the over-reaction of the patient's immune system to the threat, which doctors call septic shock.
When the body is attacked by a dangerous microbe, cells of the immune system sound the alarm by releasing cytokines - powerful chemicals with a mission to seek and destroy the invader. But some infections like E. coli and salmonella unleash such an excessive cytokine storm that the patient's blood pressure crashes catastrophically, multiple organ failure develops and death is often the result.
"It's a catastrophe that unfolds in front of your eyes," says Professor Shaunak. We do a good job of killing the bug but we do nothing to control the excessive immune response of the patient, he adds. His latest work is the culmination of 10 years research effort to address this neglected aspect of treating an infection.
The team chose to focus their research on the cytokine storm that occurs in the gut in the diarrhoeal disease shigellosis, which causes a life-threatening inflammatory diarrhoea in more than 100 million people worldwide every year. Shigella is a prime example of a microbe that tricks the patient's immune system to over-react massively. The overblown immune response causes the gut wall to rupture, allowing bacteria to invade the body.
The reaction is triggered by features on the outside of bacterial cells called LPS that are recognised by receptors on immune cells. Professor Shaunak's idea was to devise a molecular mimic that binds to the same receptors as LPS, but doesn't trigger a response. The aim would be to reduce the cytokines released to levels that would be helpful rather than harmful.
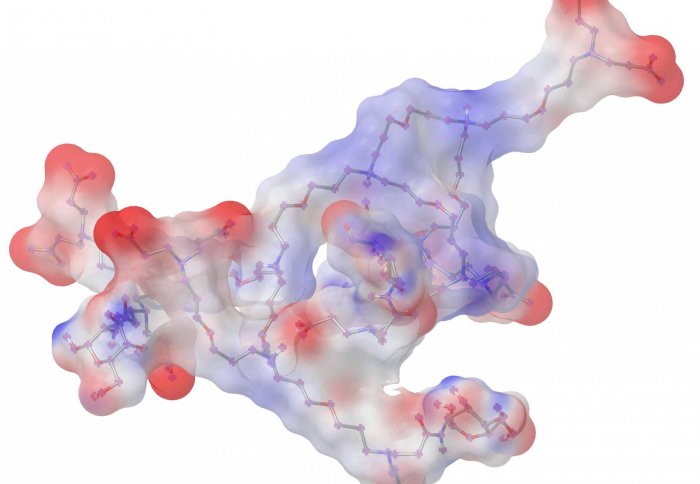
To find such a mimic, they studied products of nanotechnology called dendrimers. These molecules, whose name derives from the Greek word for tree, are made up of branches of repeating units. Dendrimers are starting to find applications as carriers for delivering drugs into cells, but Professor Shaunak sees a potential far beyond that. He believes that they could become potential drugs in their own right.
By attaching small sugar molecules to the ends of the dendrimers' branches, they made a molecule that could interact with the immune system's main detection system for bacteria. When they tested it in rabbits, they found that it protected the gut wall from the damage caused by shigella infection, and it minimised invasion by bacteria even when antibiotics were not used. The animal studies were performed in collaboration with Professor Philippe Sansonetti's group at the Institut Pasteur in Paris.
Professor Shaunak is also working with Professor Steve Matthews in the Department of Life Sciences to refine the molecule to make it easier to make on a large scale. "We are in new and unchartered waters when it comes to applying dendrimer-based-nanotechnology to infection-related-inflammation," says Professor Shaunak. "Its potential use could be much broader than the diarrhoeal disease shown in this research paper."
The study was funded by the US National Institutes of Health, the European Research Council, and EMBO.
Reference
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Sam Wong
School of Professional Development
