Study raises concerns over anaesthetic's possible link to cancer recurrence
The commonly-used general anaesthetic isoflurane increases cancer cells' potential to grow and migrate, a laboratory study has found.
Cancer often recurs after surgery, despite the best efforts of surgeons and doctors. Some studies have suggested that choice of anaesthetic might influence the chance of recurrence, but why has remained a mystery.
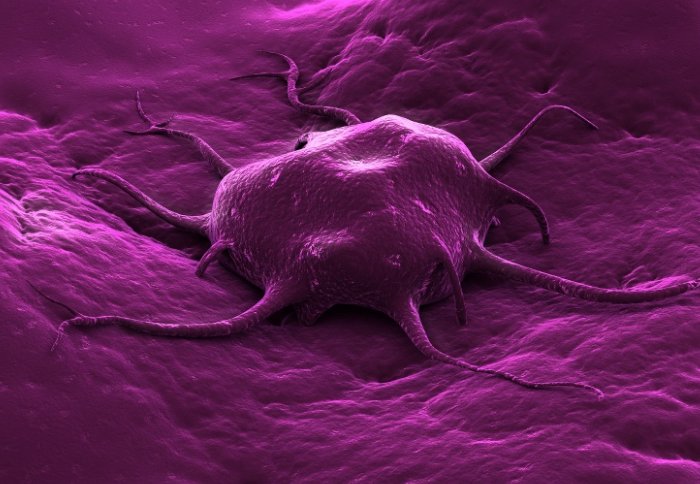
Scientists studying isoflurane’s effects on human cancer cells in the lab found that it made the cells grow and move faster. These are both hallmarks of malignancy, which means a tumour is capable of spreading around the body. The researchers are unsure if the anaesthetic has this effect in cancer patients, but if future studies show this is the case, it would suggest that isoflurane should not be used in cancer surgery.
The finding also has implications for medical research, since isoflurane is used to anaesthetise mice in cancer studies, and may affect the results of such work.
Isoflurane is one of the most commonly used general anaesthetics in the UK. Scientists have known for some time that using local or regional anaesthetic instead of general anaesthetic leads to fewer recurrences after surgery on tumours, and that different anaesthetics might be linked to different recurrence rates.
Dr Daqing Ma, from the Department of Surgery & Cancer at Imperial College London, previously showed that some anaesthetics can protect normal cells from damage caused by injury. Realising that they might also protect cancer cells in the body, his group decided to test the effect of isoflurane on human kidney tumour cells in the lab.
In the latest study, funded by a Medical Research Council PhD programme, the team applied isoflurane to the cells in the lab, then looked for signs of increased cell division and migration, and they found both. These processes are associated with faster-growing and more malignant tumours in patients.
Isoflurane seems to have this effect by activating a chemical pathway normally triggered by low oxygen levels. In cancer patients, activation of this pathway enables the growth of new blood vessels, bringing more blood and oxygen into tumours and helping them to thrive. Higher activity in the pathway is linked to poorer prognoses for patients.
“The workings of anaesthetics at the cellular and molecular levels are still largely a mystery to us, which leaves open the risk of dangerous side effects,” says Dr Ma. “This study looked at cells in the lab, so we don’t know whether the same effects are present in the body. But we do know that the choice of anaesthetic can affect clinical outcomes, and we think this needs to be investigated further.”
Dr Ma thinks the work may also have important implications for pre-clinical research using live animals. Mice are usually given anaesthetic before lab procedures to prevent their suffering – often using isoflurane. If isoflurane increases the disease potential of cancer cells, it may affect the results when new cancer treatments are tested in mice, perhaps even disguising the effects of potentially useful treatments.
REFERENCE
Benzonana et al (2013) Isoflurane, a Commonly Used Volatile Anesthetic, Enhances Renal Cancer Growth and Malignant Potential via the Hypoxia Inducible Factor Cellular Signalling Pathway In Vitro. Anesthesiology
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Press Office
Communications and Public Affairs
- Email: press.office@imperial.ac.uk
