Airport security-style technology could help doctors decide on stroke treatment
A new computer program could help doctors predict which patients might suffer potentially fatal side-effects from a key stroke treatment.
The program, which assesses brain scans using pattern recognition software similar to that used in airport security and passport control, has been developed by researchers at Imperial College London. Results of a pilot study funded by the Wellcome Trust, which used the software are published in the journal Neuroimage Clinical.
Stroke affects over 15 million people each year worldwide. Ischemic strokes are the most common and these occur when small clots interrupt the blood supply to the brain. The most effective treatment is called intravenous thrombolysis, which injects a chemical into the blood vessels to break up or ‘bust’ the clots, allowing blood to flow again.
Our new study is a pilot but it suggests that ultimately doctors might be able to use our pattern recognition software, alongside existing methods, in order to make more accurate assessments about who is most at risk and treat them accordingly
– Dr Paul Bentley
Clinical Senior Lecturer
However, because intravenous thombolysis effectively thins the blood, it can cause harmful side effects in about six per cent of patients, who suffer bleeding within the skull. This often worsens the disability and can cause death.
Clinicians attempt to identify patients most at risk of bleeding on the basis of several signs assessed from brain scans. However, these signs can often be very subtle and human judgements about their presence and severity tend to lack accuracy and reliability.
In the new study, researchers trained a computer program to recognise patterns in the brain scans that represent signs such as brain-thinning or diffuse small-vessel narrowing, in order to predict the likelihood of bleeding. They then pitted the automated pattern recognition software against radiologists’ ratings of the scans. The computer program predicted the occurrence of bleeding with 74 per cent accuracy compared to 63 per cent for the standard prognostic approach.
Dr Paul Bentley from the Department of Medicine, lead author of the study, said: “For each patient that doctors see, they have to weigh up whether the benefits of a treatment will outweigh the risks of side effects. Intravenous thrombolysis carries the risk of very severe side effects for a small proportion of patients, so having the best possible information on which to base our decisions is vital. Our new study is a pilot but it suggests that ultimately doctors might be able to use our pattern recognition software, alongside existing methods, in order to make more accurate assessments about who is most at risk and treat them accordingly. We are now planning to carry out a much larger study to more fully assess its potential.”
The research team conducted a retrospective analysis of computerized tomography (CT) scans from 116 patients. These are scans that use x-rays to produce ‘virtual slices’ of the brain. All the patients had suffered ischemic strokes and undergone intravenous thrombolysis in Charing Cross Hospital. In the sample the researchers included scans from 16 patients who had subsequently developed serious bleeding within the brain.
Without knowing the outcomes of the treatment, three independent experts examined the scans and used standard prognostic tools to predict whether patients would develop bleeding after treatment.
In parallel the computer program directly assessed and classified the patterns of the brain scans to produce its own predictions.
Researchers evaluated the performance of both approaches by comparing their predictions of bleeding with the actual experiences of the patients.
Using a statistical test the research showed the computer program predicted the occurrence of bleeding with 74 per cent accuracy compared to 63 per cent for the standard prognostic approach.
The researchers also gave the computer a series of ‘identity parades’ by asking the software to choose which patient out of ten scans went on to suffer bleeding. The computer correctly identified the patient 56 per cent of the time while the standard approach was correct 31 per cent of the time.
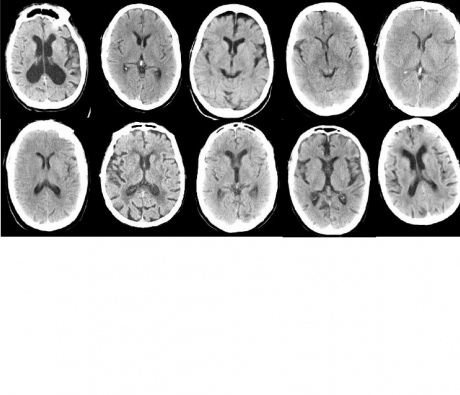
Software successfully identified which of these ten patients developed adverse outcome, outperforming radiology experts.
The researchers are keen to explore whether their software could also be used to identify stroke patients who might be helped by intravenous thrombolysis who are not currently offered this treatment. At present only about 20 per cent of patients with strokes are treated using intravenous thrombolysis, as doctors usually exclude those with particularly severe strokes or patients who have suffered the stroke more than four and half hours before arriving at hospital. The researchers believe that their software has the potential to help doctors to identify which of those patients are at low risk of suffering side effects and hence might benefit from treatment.
The study was supported through the Wellcome Trust Institutional Strategic Support Fund and the researchers have secured further funding from the Trust to conduct a larger study that will be looking at data from about 2000 more subjects across London.
-
Reference: Bentley et al. “Prediction of stroke thrombolysis outcome using CT brain machine learning.” Neuroimage Clinical. 2014. Doi: 10.1016/j.nicl.2014.02.003.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Franca Davenport
Communications and Public Affairs