Study provides vital new insight into how we produce new brain cells
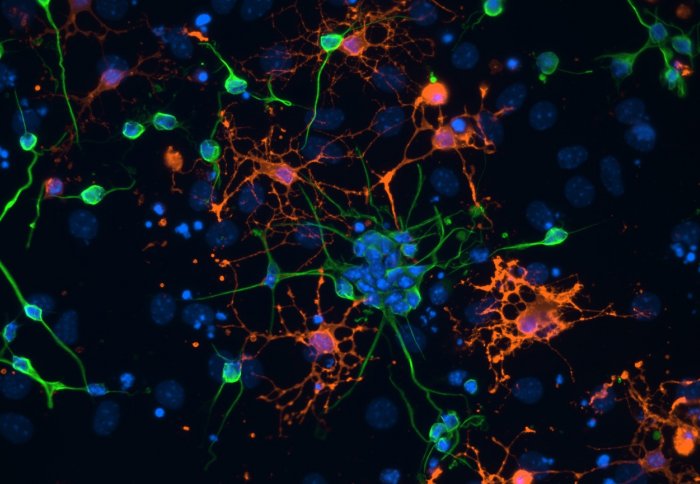
Neural stem cells differentiating into neuroblasts (green) and oligodendrocytes (red)
Researchers have identified a key mechanism in the birth of new brain cells, with implications for treating brain injury and diseases.
Neurogenesis is the process by which new brain cells are generated. The details of how and why brain cells continue to generate in adults remains a relative mystery and one that would be very valuable to solve for clinical application. It is known that the initial steps of neurogenesis involve neural stem cells dividing and specialising, but exactly how this is initiated and controlled is unclear. Neural stem cells are cells that are yet to specialise but have the potential to become neurons, which are the cells of the central nervous system.
Neurogenesis is a bit like a production line, where neural stem cells become activated to proliferate and specialise
– Dr Simona Parrinello
Junior Research Fellow
The new study, published in Nature Cell Biology, has revealed a crucial mechanism that stops stem cells from dividing or specialising when they are in direct contact with blood vessels in the brain, so that they remain in a dormant state. The hope is that if this mechanism can be blocked by medication then it could allow neural stem cells to develop into new neurons, providing a possible way to replace or repair damaged brain cells caused by brain injury, stroke or neurodegenerative diseases such as dementia.
Lead author Dr Simona Parrinello, a Junior Research Fellow and Group Head at the Medical Research Council (MRC) Clinical Sciences Centre at Imperial College London said: “Until about 25 years ago it was assumed that we only possess the neurons that we are born with, but the discovery that neurogenesis continues into adulthood has opened up a very exciting area of research with important clinical implications.
“Neurogenesis is a bit like a production line, where neural stem cells become activated to proliferate and specialise and then migrate to different regions of the brain where they become mature functional neurons,“ Dr Parrinello explained. “If we feed more stem cells into the beginning of the production line this will ultimately result in more new neurons that could help repair damage. However we need to understand the mechanisms that both start and stop the production line in order to control it effectively and put it to clinical use. In this study we have discovered a vital process that prevents stem cells developing into neurons so, if we can manipulate the process, we could potentially control the amount that go through the production line to become fully fledged neurons.”

Model of neurogenesis in the vicinity of blood vessel
The fate of neural stem cells and their potential for neurogenesis is strongly influenced by their surrounding micro-environment, of which blood vessels are a major feature. Previous research has shown that blood vessels trigger the start of neurogenesis through messages that are released from the surface of the vessels and are picked up by nearby neural stem cells. However no study has examined what occurs when the stem cells are in direct contact with blood vessels, through the ‘endfeet’ that attach to the cells on the surface of the vessels.
For the first time, the researchers studied in culture what happens when neural stem cells are in direct and stable contact with blood vessels. They observed that, even under conditions that encourage growth, the stem cells remained in the same dormant state with no division or specialisation, indicating that a mechanism was at work to over-ride any signals that might trigger their progression into new neurons. This suggests that the inhibitory process that occurs when there is direct contact with blood vessels counterbalances the process that uses messages to initiate neurogenesis.
The researchers then scrutinised in culture the signals that were responsible for maintaining this dormant state and identified two proteins in the lining of the blood vessels – ephrinB2 and Jagged1 – as being central in the signalling. They demonstrated that these proteins work in parallel to stop the division and specialisation of neural stem cells and sustain them in their original state.
The identification of the proteins ephrinB2 and jagged1 is an important piece of the puzzle
– Dr Simona Parrinello
Junior Research Fellow
Lastly the researchers investigated the effects of knocking out the genes responsible for these two proteins in mice. Once these proteins were no longer present in the blood vessels the neural stem cells started to divide, specialise and migrate to other parts of the brain. As a result this depleted the pool of neural stem cells, highlighting the importance of keeping a balance between provoking neural stem cells to develop and maintaining a sufficient store to draw upon in the future.
“The identification of the proteins ephrinB2 and jagged1 is an important piece of the puzzle, increasing our understanding of how neurogenesis occurs,” said Dr Parrinello. “Our research suggests they could be prime candidates for therapies that boost neurogenesis by blocking their activity. Compared to targeting the actual stem cells for therapy, this could provide an easier and safer treatment. Easier because the blood vessels are more accessible for intervention and safer because any changes made here are less permanent and more transient than changes made to the stem cells themselves which could modify their function more profoundly.”
The research was led by Imperial College London in collaboration with the University of Muenster in Germany and the University of Tuebingen in Germany. It was funded by the Medical Research Council and the Royal Society. Dr Parrinello holds an Imperial College London Junior Research Fellowship.
Reference: Ottone et al. ‘Direct cell-cell contact with the vascular niche maintains quiescent neural stem cells’ Nature Cell Biology, 2014. Doi: 10.1038/ncb3045
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Franca Davenport
Communications and Public Affairs