Prototype 'nanoneedles' generate new blood vessels in mice
by Colin Smith
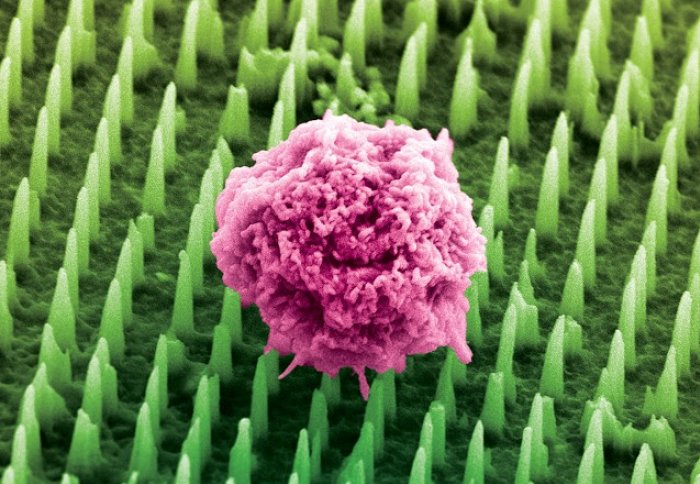
Nanoneedles delivering nucleic acids to a human cell
Scientists have developed tiny nanoneedles that have successfully prompted parts of the body to generate new blood vessels, in a trial in mice.
The researchers, from Imperial College London and Houston Methodist Research Institute in the USA, hope their nanoneedle technique could ultimately help damaged organs and nerves to repair themselves and help transplanted organs to thrive.
The nanoneedles work by delivering nucleic acids to a specific area. Nucleic acids are the building blocks of all living organisms and they encode, transmit and express genetic information. Scientists are currently investigating ways of using nucleic acids to re-program cells to carry out different functions.
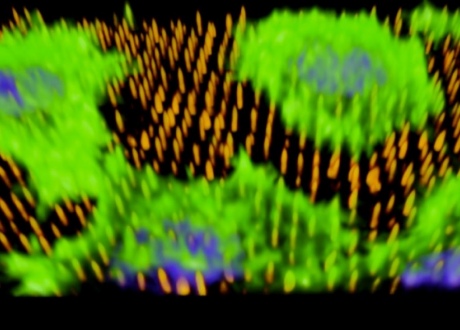
The image (above) shows human cells (green) on the nanoneedles (orange). The nanoneedles have injected DNA into the cells’ nuclei (Blue). The image was taken by the researchers using optical microscopy.
There are a number of hurdles to overcome and we haven’t yet trialed the nanoneedles in humans, but we think they have enormous potential for helping the body to repair itself.
– Professor Molly Stevens
Departments of Materials and Bioengineering
The nanoneedles are tiny porous structures that act as a sponge to load significantly more nucleic acids than solid structures. This makes them more effective at delivering their payload. They can penetrate the cell, bypassing its outer membrane, to deliver nucleic acids without harming or killing the cell. The nanoneedles are made from biodegradable silicon, meaning that they can be left in the body without leaving a toxic residue behind. The silicon degrades in about two days, leaving behind only a negligible amount of a harmless substance called orthosilicic acid.
In a trial described in Nature Materials, the team showed they could deliver the nucleic acids DNA and siRNA into human cells in the lab, using the nanoneedles. They also showed they could deliver nucleic acids into the back muscles in mice. After seven days there was a six-fold increase in the formation of new blood vessels in the mouse back muscles, and blood vessels continued to form over a 14 day period. The technique did not cause inflammation or other harmful side effects.
The hope is that one day scientists will be able to help promote the generation of new blood vessels in people, using nanoneedles, to provide transplanted organs or future artificial organ implants with the necessary connections to the rest of the body, so that they can function properly with a minimal chance of being rejected.
Professor Molly Stevens, co-corresponding author from the Departments of Materials and of Bioengineering at Imperial College London, said: “It is still very early days in our research, but we are pleased that the nanoneedles have been successful in this trial in mice. There are a number of hurdles to overcome and we haven’t yet trialled the nanoneedles in humans, but we think they have enormous potential for helping the body to repair itself.”
“This is a quantum leap compared to existing technologies for the delivery of genetic material to cells and tissues,” said Ennio Tasciotti, Co-Chair, Department of Nanomedicine at Houston Methodist Research Institute and co-corresponding author of the paper. “By gaining direct access to the cytoplasm of the cell we have achieved genetic reprogramming at an incredible high efficiency. This will let us personalize treatments for each patient, giving us endless possibilities in sensing, diagnosis and therapy. And all of this thanks to tiny structures that are up to 1,000 times smaller than a human hair.”
The researchers are now aiming to develop a material like a flexible bandage that can incorporate the nanoneedles. The idea is that this would be applied to different parts of the body, internally or externally, to deliver the nucleic acids necessary to repair and reset the cell programming.
Dr Ciro Chiappini, first author of the study from the Department of Materials, added: “If we can harness the power of nucleic acids and prompt them to carry out specific tasks, it will give us a way to regenerate lost function. Perhaps in the future it may be possible for doctors to apply flexible bandages to severely burnt skin to reprogram the cells to heal that injury with functional tissue instead of forming a scar. Alternatively, we may see surgeons first applying the nanoneedle bandages inside the affected region to promote the healthy integration of these new organs and implants in the body. We are a long way off, but our initial trials seem very promising.”
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Colin Smith
Communications and Public Affairs