Researchers develop new breath test to diagnose oesophageal and gastric cancer
by Maxine Myers
Researchers have devised a breath test that can help doctors diagnose the early signs of oesophageal and gastric cancer in minutes.
The test has produced encouraging results in a clinical study, and will now be tested in a larger trial involving three hospitals in London.
Researchers analysed breath samples of 210 patients using the test. They found that the test can discriminate between malignant and benign oesophageal cancer in patients for the first time.
The test is 90 per cent accurate and provides results in minutes, which can take up to four to six hours to process using other methods. The test can also be applied to detect gastric (stomach) cancer tumours.
According to the researchers, economic modelling showed that the test could save the NHS £145 million a year because it’s cheaper, faster and easier to perform than other methods.
Oesophageal and gastric malignancies account for 15 per cent of cancer-related deaths globally. Both cancers are usually diagnosed in the advanced stages because they rarely cause any noticeable symptoms when they first develop. As a result, the long-term survival rate is 13 per cent for oesophageal cancer and 15 per cent for gastric cancer in the UK. However, diagnosis of these cancers at an early stage can improve survival rates.
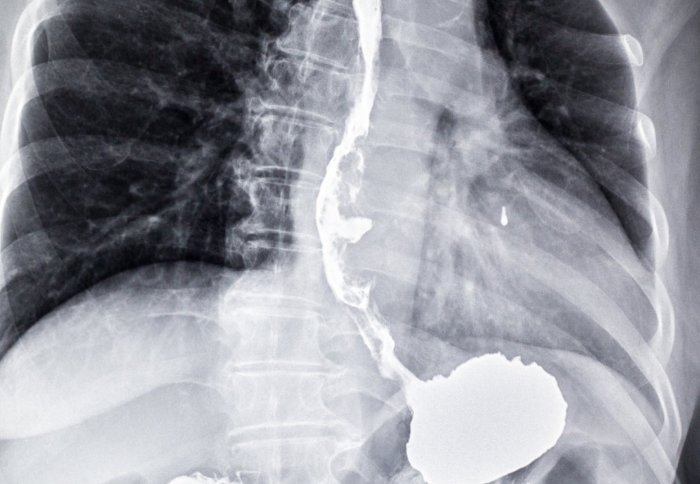
Doctors diagnose oesophageal and gastric cancers by carrying out an endoscopy. This is a procedure where the inside of the body is examined using a probe with a light source and video camera at the end via the mouth and down the gullet. However, the procedure is invasive and costs the NHS around £400-£600 per endoscopy. Only two per cent of patients who are referred for an endoscopy by GPs are diagnosed with oesophageal or gastric cancer.
The first study, published in the Annals of Surgery, was carried out by an international team led by scientists at Imperial College London and clinicians at Imperial College Healthcare NHS Trust. Researchers from UCL (University College London), Keele University Medical School, Heyrovsky Institute of Physical Chemistry and Academy of Sciences of the Czech Republic were also involved in the study.
Now, 400 patients at UCLH (University College London Hospitals NHS Foundation Trust), The Royal Marsden NHS Foundation Trust, and Guy’s and St Thomas’ NHS Foundation Trust will take part in a further trial. The researchers hope to use the findings from the clinical trial to create a sensor device that can signal to clinicians if a patient has a malignant tumour.
Professor George Hanna, lead author of the study and Director of NIHR-Diagnostic Evidence Cooperatives at Imperial College London, said:
“Oesophageal and gastric cancers are on the rise in the UK with more than 16,000 new cases diagnosed each year. The current method for detecting these cancers is expensive, invasive and a diagnosis is usually made at a late stage and often the cancer has spread to other parts of the body. This makes it harder to treat and results in poor long-term survival rates. Our breath test could address these problems because it can help diagnose patients with early non-specific symptoms as well as reduce the number of invasive endoscopies carried out on patients, which often lead to negative results. Diagnosis at an early stage could give patients more treatment options and ultimately save more lives.”
The test looks for chemical compounds in exhaled breath that are unique to patients with oesophageal and gastric cancer. The cancers produce a distinctive smell of volatile organic compounds (VOC), chemicals that contain carbon and are found in all living things, which can help doctors detect early signs of the disease. Researchers were able to identify for the first time the number of VOCs in breath samples by using a selected ion flow tube mass spectrometer, an analytical instrument used to identify what chemicals are present in a sample. This quantitative technology identified VOCs that were present at significantly higher concentrations in patients with oesophageal and gastric cancer than in non-cancerous patients. The researchers say that the results could be used to set a biomarker, a biological feature used to measure the presence or progress of a disease.
To take the test, patients breathe into a device similar to a breathalyser which is connected to a bag. The compounds in their exhaled breath are analysed by a selected ion flow tube mass spectrometer.
The researchers used breath samples of patients with oesophageal and gastric cancer at Imperial College Healthcare NHS Trust from 2011 to 2013. Patients who are at risk of developing these cancers and those who had benign tumours were also tested.
Similar breath tests to discriminate between benign and malignant tumours exist but researchers say they have lengthy processing times and are unable to quantify the amounts of VOCs present in exhaled breath.
The research was funded by NIHR Imperial Biomedical Research Centre and NIHR-diagnostic Evidence Cooperatives.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Maxine Myers
Communications Division