Airway valve treatment improves lung function
by Sam Wong
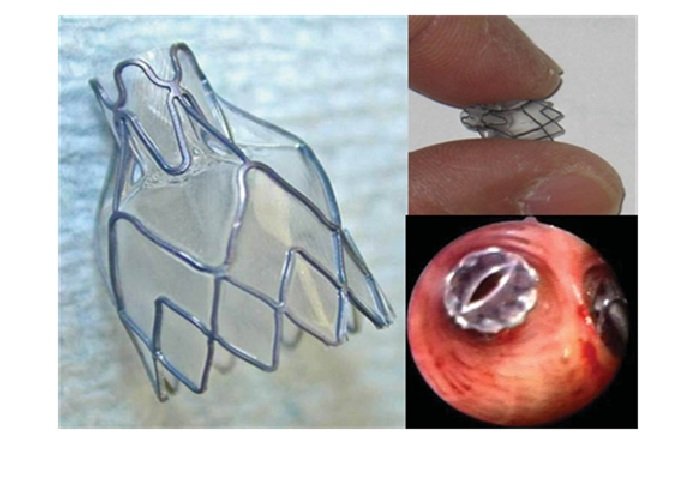
An endobronchial valve, outside the lung and (bottom right) seen inside an airway via a bronchoscope.
A study has found that using airway valves to treat people with emphysema can improve lung function and exercise capacity.
The new treatment could provide a less invasive alternative to surgery to remove the affected part of the lung.
Emphysema is a condition of the lungs that causes breathlessness, limiting patients’ ability to do even light exercise and affecting their quality of life. The condition is a form of chronic obstructive pulmonary disease (COPD), which is thought to affect more than three million people in the UK.
The progressive disease makes it difficult for patients to breathe due to damaged airways and air sacs in the lungs. Despite best treatment with standard medicines and pulmonary rehabilitation, many people with the condition experience increasing breathlessness and are limited in what they can do on a day-to-day basis.
In a new trial, at the National Institute for Health Research (NIHR) Respiratory Biomedical Research Unit at Royal Brompton Hospital and Imperial College London, doctors placed one-way endobronchial valves into the most damaged part of the lung using a thin, flexible, fibre-optic tube called a bronchoscope.
This new minimally-invasive treatment uses the valves to block off the damaged part of the lungs when the patient inhales, so the healthier areas can function more efficiently. The procedure provides an alternative for some patients to lung volume reduction surgery, which is when the most damaged parts of the lungs are surgically removed.
The trial, published today in The Lancet, involved 50 patients who had emphysema in one part of the lung and whose fissures – the separations that divide the lungs into lobes – were intact.
All underwent a bronchoscopy, where a fibre optic camera was inserted in their lungs. Half had valves placed to shut off airflow to the damaged part of their lung and half did not.
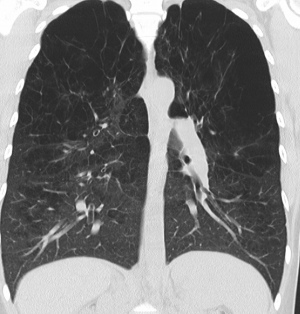
CT scan showing trapped air (black) in the lungs of an emphysema patient
Treatment with the endobronchial valves was also associated with significant improvements in exercise capacity. For example, the patients who received the valves were able to cycle on average 139 seconds longer than they could before, compared with a small decline in the control group.
Other improvements were found in breathlessness during exercise, lung volume and gas transfer, which measures how efficiently the lungs can exchange carbon dioxide for oxygen.
Dr Nick Hopkinson from the National Heart and Lung Institute at Imperial College London and Royal Brompton Hospital, who led the study, said: “The results are very exciting because they show, for the first time in a rigorous randomised controlled trial, that endobronchial valves can improve lung function and exercise capacity and achieve similar results to those seen with LVRS in properly selected patients.
“The improvement in gas transfer is of particular significance because this measure of lung function is the one most strongly associated with survival rates for COPD patients.
“A further study involving a larger number of patients is now needed to establish the best use for this technique in relation to other COPD treatments, such as lung volume reduction surgery and other novel treatments like lung volume reduction coils.”
The study was the funded by the Efficacy and Mechanism Programme, a Medical Research Council and NIHR partnership.
Reference: C. Davey et al. ‘Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial.’ The Lancet, Published Online: 23 June 2015 Open Access. DOI: http://dx.doi.org/10.1016/S0140-6736(15)60001-0
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Sam Wong
School of Professional Development