Dr Marcus Dorner - where are we in the treatment of viral hepatitis?
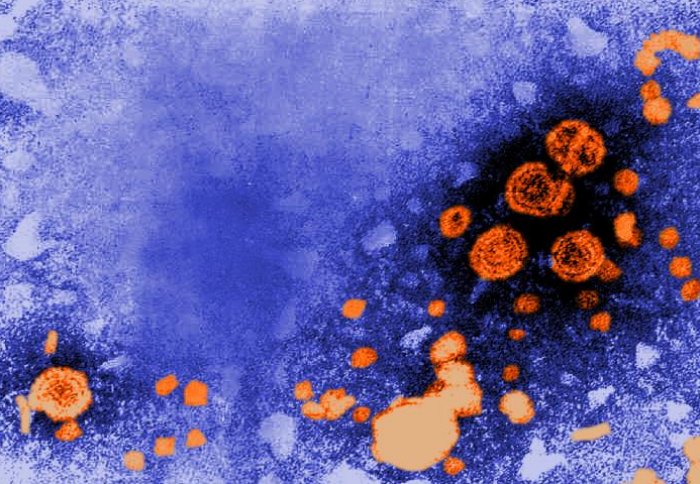
Hepatitis B virions with Dane particles. CC BY-NC-SA 2.0 Microbe World/Flickr
On World Hepatitis Day, Dr Marcus Dorner of the Department of Medicine, describes the current state of viral hepatitis research and treatment options.
Research in the field of viral hepatitis, especially on hepatitis C virus (HCV) infection has made incredible progress in recent years. This has lead to the development of an enormous number of novel therapies promising a cure for most of the over 130 million infected people worldwide (WHO 2015).
Up until recently treatment meant one year of injections with interferon, which lead to significant side effects and did by no means guarantee cure of the disease. With new therapies being approved constantly, people chronically infected with HCV can now look forward to over 90% treatment success rates, with therapies shortening in duration and virtually absent of side effects (1, 7). This has clearly changed the landscape for both the treatment of infected patients and research on HCV.
During the past few years, the focus of research and clinical virology has shifted from drug development to the identification of infected people and the optimisation of novel combination treatments. Even though the official number of people with HCV ranges from 130-170 million, there are likely many people who do not know they are infected. The slow progression of HCV together with the nature of its transmission has lead to a large number of people living with infection without knowledge of it.
For the longest time, the public has associated HCV infection with intravenous drug use and the sharing of needles; clearly contributing to the stigma associated with infection. This however is only one part of the equation. Prior to routine blood supply screening the majority of new infections could be attributed to blood transfusions, and in recent years the use of inadequately sterilized tattooing needles and dental equipment has lead to several instances of transmission of the virus. This, together with the fact that prolonged infection with HCV eventually leads to the development of liver cirrhosis and liver cancer, underlines the urgency of identifying all infected individuals and ultimately curing them.
But this is exactly the problem policy makers are facing at the moment. The efficacy and curative effects of new treatments over a relatively short period of time have in turn resulted in prices that make universal treatment prohibitively expensive. With costs as high as £120,000 for each treatment the total for treating the estimated 214,000 HCV-infected in the UK would exceed 25 billion pounds, or about a quarter of the total annual budget of the NHS (2-6). Even though pharmaceutical companies are already lowering the prices for treatments (such as the Gilead Global Access Programme) there is an urgent need for a protective vaccine, which still does not exist, as well as more economically viable treatment alternatives.
Despite the significant progress in fighting chronic liver disease associated with viral hepatitis, another member of this viral family has gone nearly unnoticed. Hepatitis B virus (HBV) shares a lot of its clinical symptoms with HCV and is also associated with the development of liver cancer. It has infected over 350 million people worldwide (WHO 2015) - over 180,000 of those in the UK (GOV.UK 2015).
Even though there is an effective vaccine available, millions of new HBV infections are reported each year. The good news for people infected is that funds allocated for viral hepatitis research will likely be re-allocated to focus on hepatitis B virus. It is however unlikely that the success story of HCV will repeat itself in the same time scale for HBV.
To date, many of the treatment options for HBV have been “borrowed” from HIV treatment, in that drugs affecting the HIV reverse transcriptase are also active in the hepatitis B virus. These treatments, although very effective in suppressing HBV replication do not constitute a cure for infection. Whenever treatment is interrupted hepatitis B virus starts replicating again. Even though in the last few years several new clinical trials were launched evaluating the efficacy of novel treatment options, a complete cure remains elusive.
It is important to keep in mind that, mainly due to the slow progression of viral hepatitis, the focus of the public is easily drawn to other infectious diseases with seemingly greater impact on public health. Globally however, the total number of people living with chronic liver disease associated with viral hepatitis is about 15 times the number of people living with HIV and the number of annual deaths are comparable to the number of people dying from seasonal influenza. These unimaginable numbers clearly mandate an even stronger effort to making effective and affordable vaccines and treatments available to everyone.
Both, hepatitis B and C virus only infect humans, making these pathogens perfect candidates for eradication; a goal that if accomplished would save countless lives in the future.
References
1. Pawlotsky JM, Feld JJ, Zeuzem S, Hoofnagle JH. From non-A, non-B hepatitis to hepatitis C virus cure. Journal of hepatology 2015;62(1 Suppl):S87-99.
2. Leidner AJ, Chesson HW, Xu F, Ward JW, Spradling PR, Holmberg SD. Cost-effectiveness of hepatitis C treatment for patients in early stages of liver disease. Hepatology 2015;61(6):1860-1869.
3. Najafzadeh M, Andersson K, Shrank WH, Krumme AA, Matlin OS, Brennan T, Avorn J, Choudhry NK. Cost-effectiveness of novel regimens for the treatment of hepatitis C virus. Annals of internal medicine 2015;162(6):407-419.
4. Chhatwal J, Kanwal F, Roberts MS, Dunn MA. Cost-effectiveness and budget impact of hepatitis C virus treatment with sofosbuvir and ledipasvir in the United States. Annals of internal medicine 2015;162(6):397-406.
5. Westerhout K, Treur M, Mehnert A, Pascoe K, Ladha I, Belsey J. A cost utility analysis of simeprevir used with peginterferon + ribavirin in the management of genotype 1 hepatitis C virus infection, from the perspective of the UK National Health Service. Journal of medical economics 2015:1-19.
6. Akpo EI, Cerri K, Kleintjens J. Predicting the impact of adverse events and treatment duration on medical resource utilization-related costs in hepatitis C genotype 1 treatment-naive patients receiving antiviral therapy. PharmacoEconomics 2015;33(4):409-422.
7. Pawlotsky JM. New hepatitis C virus (HCV) drugs and the hope for a cure: concepts in anti-HCV drug development. Seminars in liver disease 2014;34(1):22-29.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Marcus Dorner
Department of Medicine
Mr Al McCartney
Faculty of Medicine Centre