Iron levels in 60 seconds - our expert reveals the facts about the mineral
by Kate Wighton
Dr Claire Shovlin this week published research suggesting iron treatments may trigger DNA damage to cells in the laboratory, after just 10 minutes.
Although Dr Shovlin stresses extra iron can be crucial to the health of many people, she says her research suggests we need to think more carefully about the doses doctors prescribe.
Here Dr Shovlin, from the National Heart and Lung Institute at Imperial, explains why we need the mineral, and how to take iron tablets if prescribed.
Why we need iron
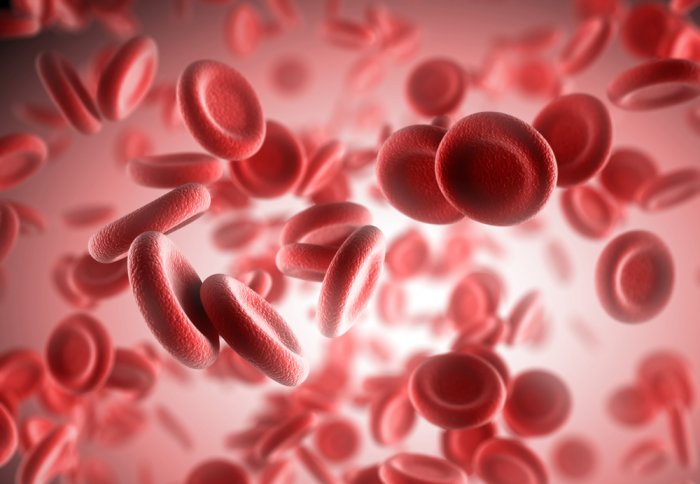
Iron is needed to make haemoglobin, the molecule in red blood cells that transports oxygen around the body. If we have too little iron we become anaemic, which triggers tiredness and lethargy. Iron is also needed in many other ways to help the body function properly.
Official recommendations state men should aim for 8.7mg of iron a day, while menstruating women should aim for 14.8 mg/day. Foods that contain iron include bread and breakfast cereals, which are fortified in the UK. Additional foods that contain iron include fish, red meat, eggs, beans and lentils.
Most diets contain around 10mg/day, and it is rare for diets to provide more than 20mg/day.
When we need more
Many people’s diets do not contain enough to meet daily needs, particularly if someone has lost iron due to bleeding, a surgical operation, or blood donation. Pregnant women also need extra iron, as the mineral is crucial for the baby’s growth and development.
However, it is recommended that extra iron is only taken on medical advice. Prescription doses of iron usually provide 65mg of iron or more in each tablet- these include tablets such as ferrous sulphate, and ferrous fumarate. About 1 in 3 people who take these tablets find they cause diarrhoea, constipation or tummy pains – but lower dosages may be better tolerated.
Dietary supplements, such as those available in chemists, are in dosages similar to the daily intake, and do not usually cause any health problems.
Take care with tea
Some food and drink can interfere with iron absorption. In the UK, one of the biggest culprits is tea – so people with low iron levels should avoid drinking tea with meals, or within an hour after eating.
There are also some medical conditions that affect iron absorption. For instance, if you have a major infection, arthritis or kidney problems your body produces increased levels of a hormone called hepcidin, that blocks iron absorption. Our genetic makeup may also affect how much iron we absorb, though this research is at an early stage.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division