Study reveals how mutations in gene CARD14 cause an increased risk of psoriasis
Research by Professor Anne Bowcock of NHLI has shown that the mutations in the CARD14 gene increase the risk of psoriasis by raised MALT1 activity.
Having previously shown that mutations in the CARD14 gene lead to psoriasis, the mechanism behind this has now been identified in a recent study by Professor Anne Bowcock and her team at the National Heart and Lung Institute, in close collaboration with Professor Steve Ley's laboratory at the Crick.
This recent research has shown that the mutations in the CARD14 gene that increase the risk of psoriasis do so via increased MALT1 activity. Furthermore, the findings suggest that MALT1 inhibitors might be used in treatment of psoriasis patients with CARD14 mutations, as well as the possibility they might be used in the treatment of more common forms of the disease.
Psoriasis is an immune condition which can effect the skin and joints. In sufferers of psoriasis the skin replacement process is sped up which leads to an abundance of skin cells. This forms itchy patches on the skin that can appear on any area of the body. Psoriasis affects around 2% of people in the UK.
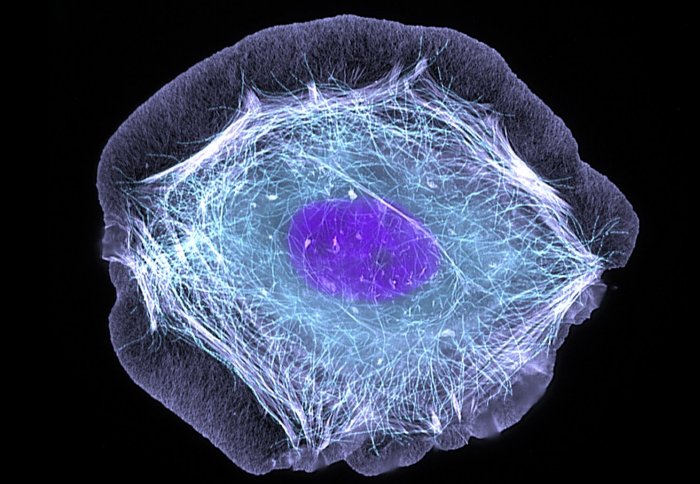
The mutations effect the CARD14 protein, which is expressed in skin cells and cells that give rise to blood vessels. They give the gene a new pattern of gene expression. In the presence of CARD14 mutations the protein is altered so that it continuously activates a molecular pathway that drives inflammation.
In this recent study the mechanisms behind psoriasis in patients with mutations in CARD14 were identified. It was discovered that MALT1 enzyme activity is switched on in these patients which increases inflammation. It was further shown that using drugs to inhibit the activity of MALT1 reduced the inflammation caused by mutant variants of CARD14.
Although these severe CARD14 mutations are relatively rare, a common genetic variant of CARD14 present in the wider population is also associated with an increased risk of developing psoriasis. This raises the interesting possibility that MALT1 inhibitors may be useful for the treatment of more common forms of psoriasis.
The study used biochemical and cellular techniques to find out more about how CARD14 mutations lead to increased inflammation in patients with psoriasis. The research group investigated how variants of the CARD14 protein affected its structure and also looked at the biological activity of the CARD14 variants in different contexts by expressing them in human skin cells, and looking at the activation of downstream signaling pathways and pro-inflammatory gene expression. Finally, they looked at the effect of MALT1 inhibitors on these signaling pathways, and showed that they disrupted them.
The paper, Psoriasis mutations disrupt CARD14 autoinhibition promoting BCL10-MALT1-dependent NF-κB activation, is published in the Biochemical Journal.
Image by ZEISS microscopy under creative commons license.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Helen Johnson
Communications Division