Scans reveal babies of mothers with gestational diabetes have more body fat
by Kate Wighton

Baby James wears special ear muffs for the MRI scanner
Babies born to mothers with gestational diabetes have more body fat at two months of age compared to babies born to healthy mothers, says new study.
Scientists from Imperial College London used MRI scanning to measure body fat in 86 babies - they took these readings shortly after birth, and again when the babies were 8-12 weeks old.
The research, published in the journal Diabetes Care, revealed that although babies born to mothers with gestational diabetes had no differences in body fat content at birth, by two months old they had 16 per cent more body fat compared to those born to healthy mothers. Most of the babies in the study were breast-fed.
Gestational diabetes is becoming more and more common. Therefore we need to understand what effects maternal diabetes has on the baby
– Dr Karen Logan
Study author
The reasons behind the differences are unknown, but possible explanations include changes in the baby's metabolism while in the womb - or even differences in the composition of breast milk in mothers with gestational diabetes.
Gestational diabetes affects around one in 20 pregnant women in the UK (and nearly one in ten in the US) and results in a woman's blood sugar levels becoming too high.
The condition, which can be controlled with diet, exercise and medication, usually starts when the woman is around seven months pregnant. Typically, it resolves soon after giving birth - though the woman may be at elevated risk of type 2 diabetes later in life.
This is the first study to show the condition causes such early changes in the baby, despite no differences at birth, explains Dr Karen Logan, lead author of the study from the Department of Medicine at Imperial:
"Gestational diabetes is becoming more and more common, and babies born to these mothers are at increased risk of developing diabetes when they grow up. Therefore we need to understand what effects maternal diabetes has on the baby.
"This new study suggests diabetes in the mother can trigger changes in the baby at a very early stage."
One of the main causes of gestational diabetes is thought to be excess weight, though other factors play a role, explains Dr Logan.
"Many of the women in our study were not overweight, and there are other possible causes of the condition, such as genetic predisposition."
She added: "All of the women in the study had their condition well-controlled, however this study suggests that even good treatment during pregnancy may not be enough to prevent longer term problems in the baby."
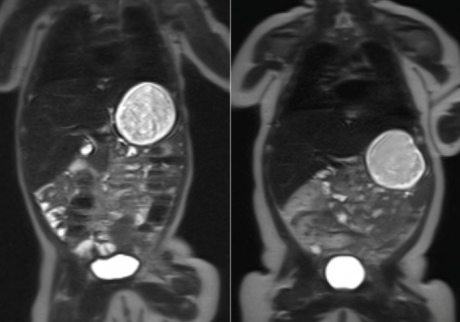 PICTURE ABOVE: MRI scans of two babies at ten weeks old. The child on the left was born to a healthy mother, while the child on the right was born to a mother with gestational diabetes. The white area on the outside of the body is fat tissue. (The large white circle in the body is milk in the stomach)
PICTURE ABOVE: MRI scans of two babies at ten weeks old. The child on the left was born to a healthy mother, while the child on the right was born to a mother with gestational diabetes. The white area on the outside of the body is fat tissue. (The large white circle in the body is milk in the stomach)
The reasons behind the difference in body fat is unknown, but theories include changes in the baby while still in the womb that trigger increased fat storage once born, alterations in the mother's breast milk, or differences in the control of appetite in the baby.
Professor Neena Modi, from the Department of Medicine at Imperial and senior author of the paper explained: "The majority of babies in our study were breast fed, and previous studies have suggested that diabetes may cause changes in breast milk - so that it contains more sugar, fat or different levels of compounds that control appetite, called hunger hormones."
The study, which was conducted at Chelsea and Westminster Hospital in London, also tracked the weight of the babies. Although babies born to mothers with gestational diabetes were found to weigh slightly less at birth, both groups of babies had a similar weight at ten weeks old.
Dr Logan said the team's next project will involve analysing the composition of breast milk from mothers with gestational diabetes. It is also unclear at this stage whether pre-existing diabetes in the mother has similar effects to gestational diabetes.
She added that if parents have concerns about their child's diet or weight they should speak to their health visitor or GP
Dr Logan said the team's next project will involve analysing the composition of breast milk from mothers with gestational diabetes. It is also unclear at this stage whether pre-existing diabetes in the mother has similar effects to gestational diabetes.
She added that if parents have concerns about their child's diet or weight they should speak to their health visitor or GP.
In the current study, which was funded by the charity Action Medical Research, the scientists scanned 42 babies whose mothers were diagnosed with gestational diabetes, and 44 babies born to mothers without the condition, as a healthy control group. The research team asked the mothers to feed the babies, and once they were asleep they were given mini ear muffs and placed in a special moulded beanbag, before going into the MRI scanner.
Dr Logan explained: "Most of the babies slept soundly during the scan, which took around 20 minutes - possibly because they found the background noise comforting. If they woke and started crying we immediately took them out of the scanner so the mum could resettle them - however this happened very rarely. The MRI technology itself is very safe - it uses no radiation and has been used extensively in previous research studies."
Lucinda Winckworth, whose son James (pictured) was in the control group of the study added: "Before James went into the scanner he was breastfed, wrapped up in a warm blanket, and had mini ear muffs placed over his ears. He fell asleep before going into the scanner, and even though I'd been warned the scanner was noisy he slept all the way through it - and all the way home! It was fascinating for us to see his scan pictures - we've kept them in his memory box, along with his ear muffs."
"Development of Early Adiposity in Infants of Mothers With Gestational Diabetes Mellitus" by Logan et al is published in the journal Diabetes Care
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division