Surgical procedure for aortic aneurysm associated with long-term mortality risk
by Kate Wighton

A minimally-invasive procedure for a serious condition may be associated with increased long-term complications, compared to an alternative op.
The research, from scientists at Imperial College London and the University of Cambridge, followed patients for up to 15 years who underwent a minimally-invasive procedure to fix an aortic aneurysm, called endovascular aneurysm repair (EVAR).
They also tracked patients with an aneurysm who underwent ‘open surgery’, which involves a large incision in the belly.
The patients who underwent the EVAR procedure had a lower mortality risk in the first six months following the operation, and were shown to have a similar mortality risk up to eight years following the operation.
These findings need to be a wake-up call to doctors across the world. Many of these aneurysms could have been caught with regularly scanning.
– Professor Roger Greenhalgh
Study author
However, the researchers wanted to then track what happened after this eight-year period.
In the latest study, published in The Lancet, the researchers found that after eight years the EVAR patients had a higher mortality rate than patients who underwent the open procedure.
The authors stress that, overall, the EVAR procedure has benefits for patients, such as less pain and a shorter hospital stay. However they urge doctors to assess patients annually following the operation, to prevent complications.
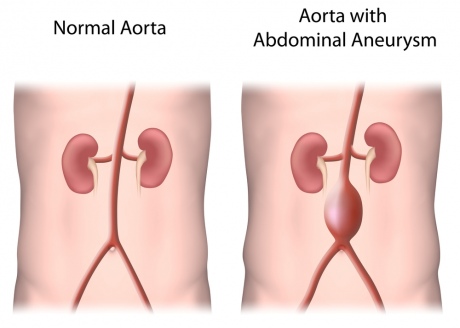
The research involved 1252 UK patients who had been diagnosed with an abdominal aortic aneurysm. This is a bulge in the aorta, the main blood vessel that runs through the body, and affects around one in 20 men over the age of 65.
If the bulge bursts it is often fatal, therefore once the bulge reaches a width of 5.5cm surgeons must operate. The EVAR procedure, which can be performed under local anaesthetic, is the most common option.
The technique involves inserting a tiny flexible plastic tube, called an EVAR device, inside the bulge to strengthen the vessel walls. The tube is inserted into the body through a small incision in the groin, and fed up to the aorta with a guide wire.
The other option is open surgery, which is performed under general anaesthetic, and involves surgeons making a large incision in the abdomen to access the aorta. A piece of man-made fibre is then used to replace the section of bulging artery.
In the longest running study of its kind, the research assessed whether one operation had advantages over the other, and randomly assigned 626 patients to have the EVAR procedure, while 626 were assigned to the open procedure. All patients were aged 60 or over (the average age was 74), and had the procedure between 1999 and 2004.
Aneurysms are often fatal if not detected before they burst
The initial results of the study suggested that in the six months immediately following the operation, patients who underwent the EVAR procedure had a 42 per cent reduction in mortality risk compared to patients who underwent the open procedure.
This was thought to be due to the complications from the open operation such as bleeding and chest problems.
The team then assessed the patients again from this six-month period to eight years after the procedure. They found no difference in mortality risk between the two patient groups.
In the latest study, the team assessed longer-term mortality risk, between 8 and 15 years after the procedure.
The patients who received the EVAR procedure were found to have a 14 per cent increased risk of mortality during this period.
They also had a greater risk of the initial aneurysm expanding again and rupturing, which in the majority of cases was fatal.
There had been 13 deaths among the EVAR patients between 8-15 years due to an aneurysm bursting. Two deaths were due to this complication in the open surgery group.
The EVAR patients were found to have a four-fold increased risk of aneurysm-related death compared to patients who received open surgery.
Professor Roger Greenhalgh, lead author from the Department of Surgery and Cancer at Imperial said these deadly aneurysms could be prevented if the patients’ aortas were scanned regularly.
He explained: “These findings need to be a wake-up call to doctors across the world. Many of these aneurysms could have been caught with regularly scanning, such as ultrasound scanning. Therefore we should be scanning patients who undergo the EVAR procedure at least once a year, rather than the current situation where patients receive scans far less often.”
He added: “The vast majority of aneurysm repairs performed in the world are EVAR procedures, and we are certainly not recommending switching back to the open operation. This involves a large incision in the body and carries serious risks."
Professor Greenhalgh explained that the aneurysms in EVAR patients seem to be re-filling when the tube inserted into the artery slips out of place. This may be because a patient’s artery continues to widen following the operation, causing the tube to eventually come loose.
“What appears to be happening is that the device inserted into the aorta can move slightly over time. This allows tiny leaks to occur. Over time, these leaks cause a pressure build-up in the original aneurysm, which is then at risk of bursting. However, if patients were regularly scanned, these aneurysms could be caught in time.”
He added that the devices used in modern procedures have improved over the last 15 years, when this study first started. Furthermore, 3D dimensional imaging has emerged to enable surgeons to fit the device more accurately, which reduces the risk of leaking.
“However, even taking these improvements into account, regular, life-long, scanning is still essential,” he said.
The team also found patients who had the EVAR procedure appeared to have a higher rate of cancer deaths in the latest follow-up period.
“We don’t know what could be responsible for this. One possibility is the higher number of CT scans these patients received, as well as the additional corrective procedures which involved radiation imaging, which is why ultrasound scans are now used. These additional cancer deaths warrant further investigation,” said Professor Greenhalgh.
He also added scientists need to investigate why some people’s artery walls seem to be more prone to widening, and developing aneurysms. Research suggests genetics may play a role, while lifestyle factors such as smoking and high blood pressure also increase risk.
Professor Greenhalgh added: “Aneurysm repair – of either type – is an essential, life-saving operation. However, any patients concerned about the operation should talk to their healthcare team, and discuss which type would be best for them, and how often they will be monitored.”
The study was funded by the National Institute of Health Research Health Technology Assessment Programme. This article presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
"Endovascular versus open repair of abdominal aortic aneurysm in 15-years’ follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial" by R. Patel et al is published in The Lancet.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division