MRSA uses decoys to evade a last-resort antibiotic
by Kate Wighton
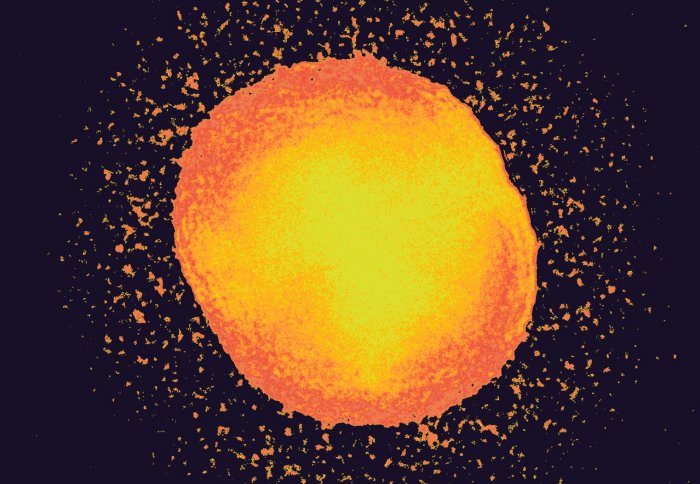
An MRSA cell releases decoys, allowing it to evade an antibiotic
The superbug MRSA uses decoys to evade a last-resort antibiotic, reveals new research.
The findings, from scientists at Imperial College London, suggest potential new ways of tackling the bacteria, such as interfering with the decoys.
Methicillin-resistant Staphylococcus aureus (MRSA) is responsible for thousands of deaths around the world each year. However, because the bacteria are resistant to many different antibiotics, treatment options are limited, and often ineffective.
One of the few antibiotics that can be used against MRSA is a drug of last resort known as daptomycin. However nearly a third of MRSA infections are not cured by this drug, leaving patients with a poor prognosis.
These fat molecules act in a similar way to the decoy flares released by fighter planes to avoid a missile.
– Dr Andrew Edwards
Study author
But until now scientists didn’t know how MRSA managed to survive daptomycin treatment.In the latest findings, published in the journal Nature Microbiology, a team from Imperial discovered that MRSA releases decoy molecules that allow them to escape being killed by the antibiotic. The decoys are made of the same type of fat that make up the outer layer of MRSA cells. The antibiotic usually latches onto this fat layer, before drilling a hole through the outer shell and killing the bacteria.However, when MRSA releases these fatty decoy molecules the antibiotic latches onto these instead, and is deactivated.
Dr Andrew Edwards, lead author from the Department of Medicine at Imperial, explained: “These fat molecules act in a similar way to the decoy flares released by fighter planes to avoid a missile. The antibiotic mistakenly targets the decoys, allowing the bacteria to evade destruction. This is the first time this decoy system has been seen in MRSA.”
Using bacterial cells in the laboratory and mouse experiments, the scientists discovered that only some MRSA bacteria can use this decoy system. The team believe this is why around 30 per cent of infections are not cured by the antibiotic daptomycin.
In these resistant infections, the MRSA bacteria turn off a communication system they normally use to ‘talk’ to each other. This communication system allows the bacteria to release toxins that damage human cells. However, this system also seems to interfere with decoy production.
Dr Edwards, who is based at the Medical Research Council’s Centre for Molecular Bacteriology and Infection at Imperial, explained: “These MRSA bacteria ‘go dark’ and stop all communication. It is the switching off of this communication system that allows the decoys to work so effectively.”
He added: “Our focus now is on understanding more about how these decoys are made and how they can be shut off completely to help daptomycin work better in patients.”

Dr Andrew Edwards is now studying how to switch off the MRSA decoys
Dr Edwards said that a similar decoy mechanism has been seen in E. coli bacteria.
“Our findings suggest we may have underappreciated the importance of this decoy system, and that it probably exists in many other bacteria.”
Further experiments revealed the release of decoys can be partially prevented using a second antibiotic, similar to penicillin, called oxacillin. Although MRSA is resistant to oxacillin, using it alongside daptomycin may allow the latter antibiotic to kill the bug more effectively. Previous research has suggested penicillin-type antibiotics help daptomycin to kill MRSA – although scientists didn’t know why. A clinical trial using the two antibiotics, led by an Australian team, is currently now underway.
Furthermore, tests revealed that a next generation antibiotic, currently in clinical trials, seems to stop production of the fatty decoys.
“This suggests this new antibiotic may also help daptomycin kill MRSA – which could provide another treatment option for patients” added Dr Edwards.
Dr Jonathan Pearce, head of infections and immunity at the Medical Research Council, which supported the work, said: “In the fight against antimicrobial resistance, we are desperately searching for new ways to treat bacterial infections like MRSA as they dangerously start to become resistant to even last resort antibiotics. This study has uncovered a rather cunning tactic that these and possibly other bacteria use to evade current treatment, and armed with this new knowledge, we can begin to develop new and improved treatments to help tackle what is one of the biggest threats to global health.”
Professor Melanie Welham, Chief Executive of the Biotechnology and Biological Sciences Research Council, added: “This demonstrates the value of research that explores the frontiers of chemical biology in bacteria. Finding the biological mechanisms behind why antibiotics do and don’t work is crucial in the fight against anti-microbial resistance.”
The work was supported by the Medical Research Council, the Biotechnology and Biological Sciences Research Council (BBSRC) and the Wellcome Trust.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division