New insight on how cells replicate and the implication on new cancer drugs
Research offers a new crucial piece of understanding on how cells choose whether to replicate or not.
Research published today in Nature communications offers a new crucial piece of understanding on how cells choose whether to replicate or not and the implications it could have on new cancer drug discovery. Sam Cooper, (STRATiGRAD PhD student in the Division of Computational and Systems Medicine) worked with a researcher from the Institute of Cancer Research and a mathematician from Oxford University on combining expertise and techniques to form these advances. Sam speaks about how this collaboration began and the implications of their findings.
What was the problem you were looking at?
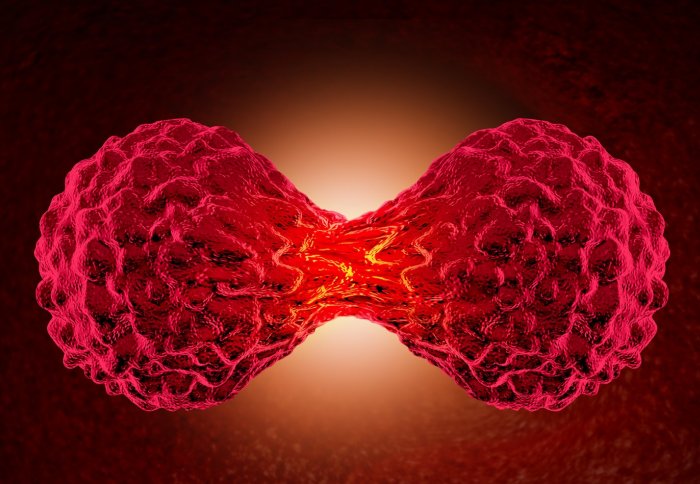
The cells in our body need to grow and replicate, in order for us to remain healthy. However, if cells replicate with damaged DNA they risk propagating this to future generations which may cause cancer. As such, cells have evolved mechanisms to prevent replication in the presence of DNA damage.
We know this mechanism involves the accumulation of a molecule p53 in response to DNA damage that produces a protein called p21, which blocks cells from replicating. Yet, we don’t fully understand the dynamics of how this mechanism works; this is like finding the parts of an engine, without knowing how they move to power a car.
Work in live cells by Galit Lahav and colleagues has shown that p53 levels pulse in response to DNA damage, this representing the first part of the mechanism. We hypothesised that p21 levels increase over time after each pulse of p53 and that once high enough then block replication, this being the second part of the mechanism coupling DNA damage to a block on replication.
How did you get involved with this research project and what part did you play in it?
In my research as a PhD student I develop machine learning techniques to automatically study images of cells. I realised the software I develop could be adapted to study live cells. Alexis Barr was working at the Institute of Cancer Research, studying p21 in live cells but couldn’t analyse all the vast quantity of data she was producing. By adapting my software we could analyse all of this data, and working together with a mathematician from Oxford University, the three of us discovered the reset mechanism and validated the original hypothesis.
Finally our work demonstrated the existence of a second mechanism that delays cell replication giving cells more time to sense DNA damage, yet what this mechanism is remains an open question that we’re now seeking to answer. Identifying the components of this mechanism would also provide a crucial new avenue for cancer drug discovery.
How did you do it?
The use of a fluorescent p53 reporter protein to measure its levels in live cells revealed that it emits pulses of activity in response to DNA damage. We therefore took the same approach to study p21 dynamics, by linking p21 to a fluorescent reporter protein.
However, unlike the live p53 studies which looked at the short term effect of DNA damage, we wanted to establish the effect of p21 on replication block which may take several days. We therefore needed to image cells over much longer periods of time. This meant developing new machine learning techniques to automatically track and extract data from these living cells.
With these new tools, we then imaged 1000’s of cells over time periods lasting several days. Analysing this data confirmed our hypothesis that DNA damage and p53-signalling cause an increase in p21 over time, and if these levels climb high enough cells stop replicating. Importantly, our work also found a novel mechanism by which cells reset p21 levels if DNA damage levels are not high enough to stop replication.
What are the implications of you findings?
By confirming our hypothesis on how p21 dynamics couple p53 signalling to blockade of cell replication, we have added a new crucial piece of understanding to the puzzle of how cells choose whether to replicate or not. Moreover, in many cancer cells where p21 levels are high, the proteins behind the reset mechanism we defined are often upregulated. If we could target this mechanism with drugs we could selectively prevent these cancer cells from replicating and even cause them to die. This could provide new treatments against cancer cells that express p21 which are often particularly resistant to clinical treatments such as chemotherapy and radiotherapy.
Main funding behind this project was a BBSRC Strategic LoLa grant (BB/M00354X/1)
Find out more:
“DNA damage during S-phase mediates the proliferation-quiescence decision in the subsequent G1 via p21 expression” published in Nature communications.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kathryn Johnson
Department of Surgery & Cancer