One donor's support to improving health in Africa

Individuals can make a huge difference to the health of the poorest people in Africa.
Bill and Melinda Gates, through their foundation, are a shining example, having invested billions of dollars, since 2000, helping the World Health Organisation (WHO) and a number of non-governmental organisations (NGO’s) to improve the health of hundreds of millions of children and adults across Africa and other developing countries. Few philanthropists are as wealthy, though many are as committed to supporting cost-effective health interventions, like treating and protecting populations against the life destroying effects of neglected tropical diseases (NTDs), in the hope of achieving the WHO’s Sustainable Development Goals.
The Schistosomiasis Control Initiative (SCI) specialises in reaching children and adults infected with the NTDs schistosomiasis (bilharzia) and intestinal worms (hookworm, roundworm and whipworm). The initiative provides technical assistance to Ministries of Health and Ministries of Education to develop the necessary in-country infrastructure to deliver national treatment programmes against these worm infections through health centres and schools, with the direct result of improving the health, quality of life and education of the poorest people, particularly in sub-Saharan Africa.
Luke Ding, with his background in finance, was attracted to the growing movement of effective altruism focusing on using evidence and careful analysis to do the most good. Leading this movement is the charity evaluator GiveWell and the Centre for Effective Altruism, both of which strongly advocate for support to SCI.
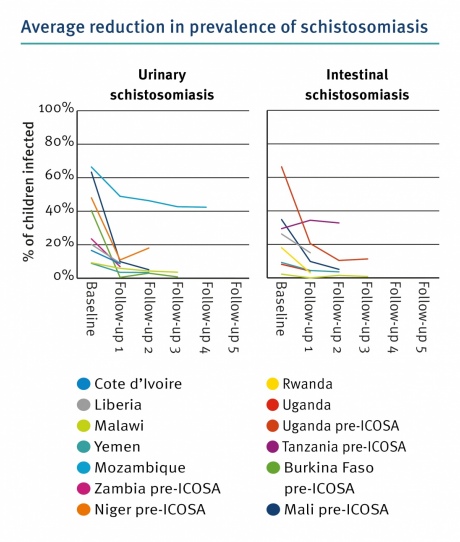
In 2011, Luke made his first donation to SCI of £800,000 to support the national NTD programme in Burundi. He continued to support the programme in Burundi, donating a further £775,000 during the following two years. Burundi has a population of 11 million people, of which 3.5 million are of school-age. Prevalence of intestinal worms was very high and 10% of the population were infected with or lived in high risk areas for schistosomiasis. The programme had been running successfully for several years but funding had run out. Luke’s donation secured the programme’s survival. With Luke’s financial support, SCI assisted the government to deliver 2,629,708 treatments to children and at-risk adults for schistosomiasis and 27,446,413 treatments to children and at-risk adults for intestinal worms over a 5-year period (2011-15). The impact of these treatments was very marked, with prevalence of infections being significantly reduced and more importantly only low-grade infections detected in children, which carries radically less risk of serious symptoms of the disease developing.
In 2014, at the encouragement of Professor Alan Fenwick, Luke increased his financial commitment to SCI even further, when he donated £197,160 to fund a pilot programme in Madagascar. Madagascar has the fifth highest rate of schistosomiasis in the world and 107 of the country’s 114 districts are endemic for schistosomiasis. With a population of 22 million, over 50% of school-age children (SACs) in many districts are infected with schistosomiasis which requires annual treatment. In some districts, up to 41% of SACs are heavily infected with schistosomiasis. Having funded the pilot programme in its entirety, he donated a further £685,000 via the UBS Optimus Foundation to fund the programme’s expansion, with the aim of achieving national coverage. In the first 3 years of the programme, 2,921,251 treatments for schistosomiasis have been administered and 1,404,205 for intestinal worms. Average cost per treatment in FY2015-16 was £0.27. The programme continues to grow but requires additional funding in order to achieve national coverage.
In addition to supporting treatment programmes in Burundi and Madagascar, Luke has also provided financial support and advice on central operations to SCI management.
In 2017/18, SCI will support 16 countries in sub-Saharan Africa and Yemen to deliver treatments for schistosomiasis and intestinal worms to over 40 million children and at-risk adults with the resulting impact of improving nutritional status, stopping/reversing the damaging effects of these infections, protecting children from serious health consequences, increasing school attendance by up to 25%, and increasing future earnings by 40%.
Extract from the impact analysis provided to DFID for the ICOSA Programme:
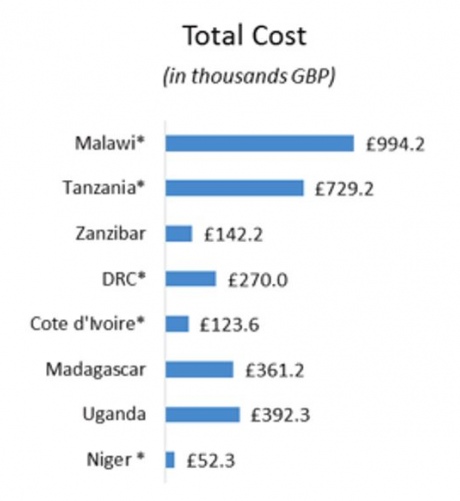
Cost per treatment overview (FY6: 2015-16):


Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Mrs Alexandra Grainger
School of Public Health