Researchers to investigate screening for prostate cancer using MRI
by Ryan O'Hare
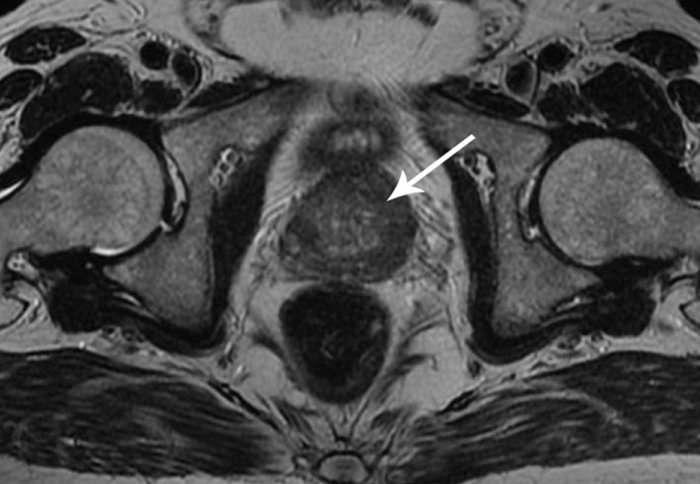
An MRI scan of prostate cancer
A new clinical study will test for the first time if MRI scans can be used for population screening to detect prostate cancer more accurately.
The current prostate-specific antigen (PSA) test is considered too unreliable for population screening, but researchers will investigate whether MRI could be used to screen men to pick up cancers earlier and more reliably, potentially helping to save lives.
They will also study whether, combined with cutting-edge techniques such as genomics and machine learning, MRI scans can replace prostate biopsies.
Prostate cancer patients advising the study say they are particularly excited by the prospect of large reduction in biopsies, as they have serious side effects in the majority of patients, which include pain, bleeding, infections leading to sepsis, and urine retention.
A group, led by Professor Mark Emberton at University College London – in partnership with King’s College London, Imperial College London and at least 12 industry partners – aims to recruit 1000 men with medium to high risk cancers to find out if MRI can be combined with other high-tech diagnostic tests to predict cancer progression.
New research
The new study is being launched with funding of £4.1m from the Medical Research Council (MRC) and £1m from Cancer Research UK. The ultimate aim of the research is to develop tests that are better than biopsies for targeting the right cancer treatment to the right person (including determining if they don’t need treatment).
It builds on a ground-breaking study led by Professor Emberton and colleagues, published in The Lancet last year, which reported that MRI scans for men who had a positive PSA test could rule out prostate cancer in 27% of the men tested, meaning they could avoid having a biopsy. They also found that for men with a possible tumour, the MRI scan could be used to direct the biopsy needle to the right location, so 18% more cases of serious prostate cancer were detected.
Professor Hashim Ahmed, Chair of Urology at Imperial College London, said: “Using MRI to screen for prostate cancer has the potential to detect and diagnose cancers at a much earlier stage. We hope this study will tell us whether the positive results seen in smaller trials can now be replicated in a larger cohort, providing the evidence needed to apply the technique in clinical practice.”
Professor Emberton said: “Our recent studies have begun to show how MRI technology will transform prostate cancer screening and diagnosis. Now we’re starting an ambitious new study, to combine MRI with the latest technologies – such a machine learning on MRI images and detecting DNA shed by cancers in blood – to see if we can find a way to make prostate cancer testing more reliable and maybe even do away with the need for biopsies altogether. We want to use MRI combined with new diagnostic tests to predict how the cancer will progress and to target the right treatment to the right person.”
Existing tests
Currently, the PSA blood test for prostate cancer is considered too unreliable to be used for population screening in the UK: about 75% of men who get a positive result are not found to have cancer (a false positive), and it misses the cancer in about 15% of men with prostate cancer (a false negative).
In the study, researchers will also be taking the MRI test out into the community for the first time to see how well it detects prostate abnormalities in 300 men aged 60 to 75 who have never had a PSA test.
“We will be testing if the MRI can be used for screening men and we hope that it will detect serious cancers earlier that are currently missed,” explained Professor Emberton. “If we can detect cancers earlier and more reliably with a non-invasive test, this could help to improve the survival rates to prostate cancer, which kills about 11,800 men in the UK annually.
“MRI scanning for prostate cancer could also help a quarter of a million men, maybe up to half a million men a year, to avoid an unnecessary biopsy if the MRI is negative. The majority of men will be reassured they don’t have prostate cancer and importantly they may be able to avoid the harms of a biopsy, plus healthcare systems will be able to avoid the costs. MRI is the perfect tool because it’s relatively cheap, widely available and reliable.”
This article is adapted from materials supplied by the Medical Research Council.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ryan O'Hare
Communications Division