Molecular ‘rabble-rouser’ fuels pancreatic cancer growth
by Kate Wighton
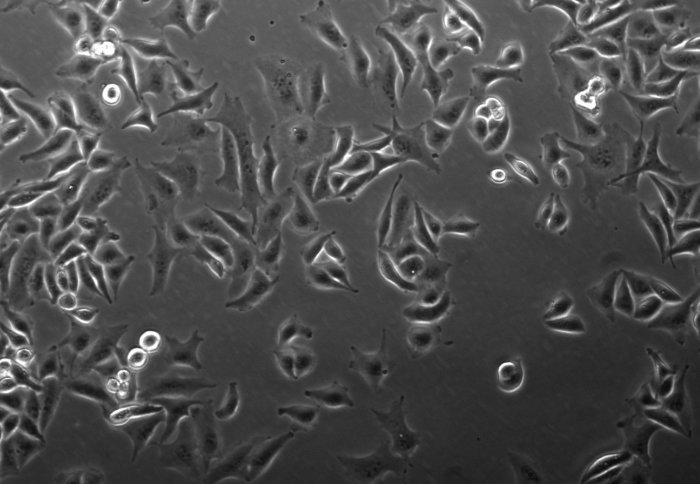
Aggressive pancreatic cancer cells
A type of molecular ‘rabble-rouser’ that triggers pancreatic cancer to become aggressive and spread around the body has been identified by scientists.
The team behind the early-stage research, led by Imperial College London and funded by Action Against Cancer and Pancreatic Cancer UK, say the findings may open avenues for treatments that target these molecules.
The molecules, called microRNAs, could also potentially be used to assess how aggressive a patient’s cancer is, and how likely it is to spread around the body.
The cells become further apart from each other – they are spiky, angry, and want to go everywhere in the body and cause trouble Dr Silvia Ottaviani Study author
Around 10,000 people are diagnosed with pancreatic cancer every year and the disease has the lowest survival of all the 20 common cancers, with less than seven per cent of patients surviving beyond five years.
In the latest research, published in the journal Nature Communications, scientists discovered that two microRNAs called miR-100 and miR-125b, work together with a molecule called Transforming Growth Factor Beta (TGF-b) to promote growth and spread of pancreatic cancer.
MicroRNAs help control which genes are switched on and off in a cell. They have previously been implicated in cancer, as they can turn on genes that make cells cancerous.
Calming a cancer cell
By using the cutting-edge CRISPR techniques, the team generated cells lacking the part of the DNA required to produce these microRNAs.
Interestingly, the team showed that these cells, when no longer able to produce these microRNAs, switched back to a less aggressive behaviour. In addition, they showed TGF-b alone was no longer effective in driving tumour growth and spread. The team further validate these findings in mice models, where cells lacking these microRNAs injected into mice formed less tumours, and were less likely to spread to other areas of the body.
They then studied tumour samples from around 100 patients with pancreatic cancer and scanned these tumours for levels of the two microRNAs. The scientists found that aggressive tumours – which are more likely to prove fatal and spread around the body, contained higher levels of the microRNAs.
They then analysed patient survival, and found that patients with high levels of these molecules had worse survival rates.
Further experiments revealed these microRNAs affect a number of genes that trigger chaos in the cell, and lead to aggressive cancer. These genes are associated with uncontrolled cell growth, DNA damage and cell movement.
Test could reveal best treatment
Dr Silvia Ottaviani, joint first author of the paper from the Department of Surgery and Cancer, explained: “These molecules act like the ‘rabble-rousers’ in tumour cells – they drive a number of processes that cause cancer cells to become aggressive, and more likely to invade other areas of the body. We see this when we look at the cells under a microscope – they become elongated and further apart from each other – they are spiky, angry, and they want to go everywhere in the body and cause trouble.”
The team are now planning further investigations on these two microRNAs, added Dr Ottaviani.
“We now need to find out if stopping the production of these molecules will slow pancreatic cancer growth, or make the cancer cells easier to kill with chemotherapy. We are also looking at whether these molecules could one day form a type of test allowing doctors to gauge how aggressive a patient’s cancer is, which would help them decide the best treatment options.”
Reducing death rate
Dr Ottaviani pointed out that most of the patient samples were obtained from pancreatic cancers that had spread to lymph nodes and nearby tissues and the team is now hoping to study more advanced and metastatic tumours in their next experiments.
Professor Justin Stebbing, joint first author from the Department of Surgery and Cancer at Imperial, added: "This groundbreaking work helps explain why some genes are turned on and off in cancer stem cells, via new molecules called long non-coding RNAs, and this will help in our understanding of how to eradicate them, increasing the cure rate and decreasing the death rate from cancer."
The work was supported by Pancreatic Cancer UK and Action Against Cancer
-
"TGF-β induces miR-100 and miR-125b but blocks let-7a through LIN28B controlling PDAC progression” by S. Ottaviani et al. is published in Nature Communications
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division

