How a gene linked to obesity could provide new insights into diabetes
by Ryan O'Hare
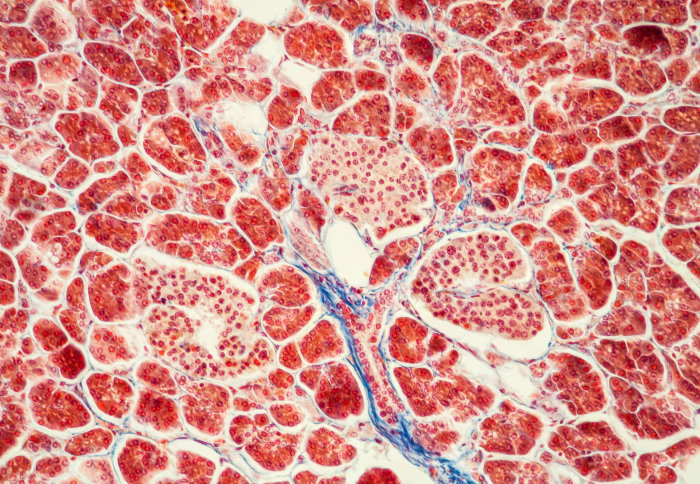
A gene linked with obesity affects how pancreatic cells (pictured) processes insulin
A gene previously linked with obesity has been found to affect how the body processes insulin, with potential implications for some forms of diabetes.
Scientists have uncovered a number of genes which may play a role in obesity and metabolism. Previous studies suggested that variations of one of these, a gene called neuronatin (Nnat), may have a link with weight gain in children.
Now, researchers have shed more light on this lesser known gene, uncovering a new mechanism for how it affects metabolism.
Through a series of studies with mice and human pancreatic cells they found that loss of this gene does not result in marked changes to how much food animals eat. However, it does affect how cells in the pancreas process insulin.
According to the group, led by researchers from Imperial College London, the findings may have implications for people with rare forms of diabetes.
Cellular mechanisms
In a paper, published in the Journal of Clinical Investigation, they explain that Nnat helps to regulate how cells sort and send proteins, such as insulin, to where they are needed.
To study its effects, researchers used genetically modified mice in which Nnat had effectively been ‘switched off’.
The researchers noticed that when the animals were given glucose they were unable to produce enough insulin to restore their blood sugar to healthy levels.
This gene appears to be involved in the efficient processing of a signal peptide for insulin Professor Dominic Withers Study author
Insulin is made up of short protein chains, produced by specialised cells in the pancreas, called beta cells. But in order for it to become active and transported to where it is needed it must be edited –and a short piece snipped off – via a process called signal peptide processing.
The team found that this editing process was reduced in mice lacking Nnat compared with healthy mice, which led to less of the hormone being stored and released by the beta cells.
Professor Dominic Withers, Clinical Chair in Diabetes & Endocrinology at Imperial and lead author, said: “This gene appears to be involved in the efficient processing of a signal peptide for insulin – so that's the reason why cells don't secret and produce enough of the hormone.”
He added: “We've studied these animals in a lot of detail and the predominant effects are upon insulin secretion and the handling of glucose as opposed to the regulation of feeding and bodyweight”
Rare forms of diabetes
According to the team, their findings may help to shed more light on rare forms of diabetes, where a mutated form of insulin is produced but is not effective as it cannot be properly processed. In some forms of diabetes, the build-up of insulin in the pancreas can become toxic, leading to permanent damage to the cells and diabetes.
Dr Steve Millership, the first author on the paper said: “These findings also highlight the potential importance of ‘imprinted genes’, where the activity of a gene originates solely from one parent – with the paternal form of Nnat strongly expressed. They may explain that the way in which this imprinted gene affect metabolism may give insights into the specific contribution of a mother’s or father’s genes to metabolic disease in their children.”
Professor Withers concluded: “This study shows that at least in mice Nnat does not have a profound effect on feeding and bodyweight, but understanding its subtle effects on metabolism are important.
“There are forms of human diabetes in which the body produces enough insulin, but something in the way it is processed goes wrong.
“By better understanding the cellular mechanisms at play, we are laying the groundwork on which future therapies to treat the disease may be discovered.”
-
‘Neuronatin regulates pancreatic beta cell insulin content and secretion’ by Steven Millership et al. is published in the Journal of Clinical Investigation.
Image: Shutterstock / Dr Norbert Lange
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ryan O'Hare
Communications Division