New strategic research centre launched to combat infection in Cystic Fibrosis
Research to look at how personalised medicine can be used to treat cystic fibrosis infections.
Professor Jane Davies is to co-lead a Strategic Research Centre (SRC) that has been awarded a grant of £750,000 from the Cystic Fibrosis Trust, one of two recently awarded, in a bid to start a new era of research via investment in ‘personalised medicine’. Professor Davies of the National Heart and Lung Institute will be leading a team exploring a ‘Personalised approach to Pseudomonas aeruginosa infection’. The lead co-investigators are Dr Huw Williams, Professor Alain Filloux and Professor Zoltan Takats from Imperial College London, Professor Jeremy Webb from the University of Southampton, and Anke-Hilse Maitland van der Zee from the University of Amsterdam.
"Just as no two patients are identical, the bacterial strains harboured by patients are also different, either in their genes or their behaviours." Professor Jane Davies
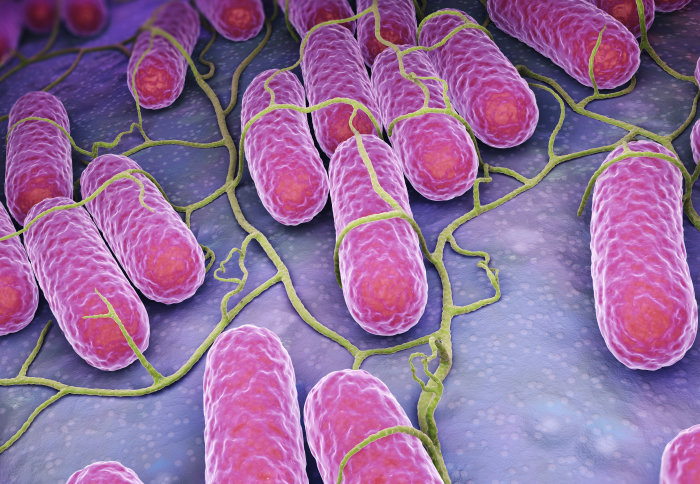
Pseudomonas aeruginosa bacteria are a common cause of lung infections of cystic fibrosis patients, and their resilience makes the infection hard to treat. That is why Professor Jane Davies and her team have been looking for new ways to tackle the bugs. In her previous SRC, Jane and her team found a large variation in how different strains of the bacteria live in the lungs of people with cystic fibrosis. These different strains can make a big difference to whether Pseudomonas becomes established in the lungs and how easy it is to treat.
At present many healthcare treatments are a one-size-fits all affair, where an approved treatment is applied in the same way to all patients. The idea of personalised medicine is that we can start to better match a treatment to an individual patient, by looking at things like a person’s genes or perhaps the strain of an infection that we are dealing with. The latest award will help the team to investigate better ways to detect Pseudomonas and understand how it settles in the lungs on a strain-by-strain basis, as well as to develop more effective drugs for treating it.
Professor Davies said: “We are delighted to have been granted Personalised Medicine SRC funding to build on the achievements of the collaboration established from our first award. Just as no two patients are identical, the bacterial strains harboured by patients are also different, either in their genes or their behaviours. Understanding these differences, and their implications for treatments, could substantially reduce the detrimental effect Pseudomonas has on someone’s lung health.”.
For someone living with cystic fibrosis the first step is detecting the presence of an infection. The researchers will be looking at methods for rapid and easy detection of Pseudomonas, looking for its presence in the most easy-to-collect way possible. Working with industrial and academic collaborators, Professor Davies and her colleagues at Imperial and the University's of Southampton and Amsterdam, will be looking at ways of detecting traces of the bacteria in the patient’s breath – a method which sounds simple, but despite several research attempts, is not available as a clinical tool.
Pseudomonas adapts to living in the lungs of people with cystic fibrosis and employs various defensive strategies to thwart treatment. An important aspect of the new SRC is to understand these strategies better, and spot any differences in strategies between different strains. Ultimately, this detailed understanding will lead to the development of more effective treatments. The new research is due to start in September this year and will run for three years. The SRC was established as a fully collaborative structure; the team will welcome ideas for joint projects and requests for clinical bacterial isolates from academic colleagues in Imperial and further afield.
This article is based on materials provided by the Cystic Fibrosis Trust – read the news on their website.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Helen Johnson
Communications Division