What happens when our cells stop cleaning up after themselves?
A cell needs to get rid of its waste proteins effectively in order to function – but what happens to our bodily tissue when this system breaks down?
It's a question that’s been relatively unexplored until now. There is a good understanding of what happens inside the cells themselves when chronic disruption of proteostasis occurs – i.e. the cellular process that keeps proteins working properly – but next to nothing is known about how this affects tissue in the body. This is despite the fact that the issue is linked to a long list of diseases – notably Alzheimer’s, Parkinson’s, diabetes and cancer.
A team of researchers led by Dr Holger Auner (Department of Medicine, Imperial College London) and Dr Eileen Gentleman (King’s College London) decided to investigate further. Taking a materials science-based approach, they used cells to engineer a unique model of bone-like tissue in the lab. In doing so, they were able to see for the first time how disrupted proteostasis impacted on the tissue’s physical properties.
They focussed on two major components of the cellular protein waste disposal system: VCP/p97 and the proteasome. While they found that obstructing the proteasome slightly enhanced the formation of tissue, they saw a remarkably different effect on their lab-made “mini bones” when they inhibited VCP/p97: the tissue was softer, contained less protein, appeared to have more crystalline mineral, and seemed to have abnormal traits in certain parts of its structure. Significantly, this could help to provide a fuller picture of how diseases that target the same part of the cell’s protein breakdown machinery play out within the body.
The findings also provide a new lens for assessing future treatments; a number of different components, including VCP/p97, are currently being investigated as anti-cancer drug targets. By taking a closer look at how changes in proteostasis affect our bones, the study highlights potential unwanted skeletal effects that might be caused by such treatments. As such, the team now hope that their model could in future provide a platform for testing out new therapies at an early stage, and allow researchers to easily detect and quantify changes in tissue.
‘An engineered, quantifiable in vitro model for analysing the effect of proteostasis-targeting drugs on tissue physical properties’ by Sandra Loaiza, Silvia A.Ferreira et al., is published in Biomaterials.
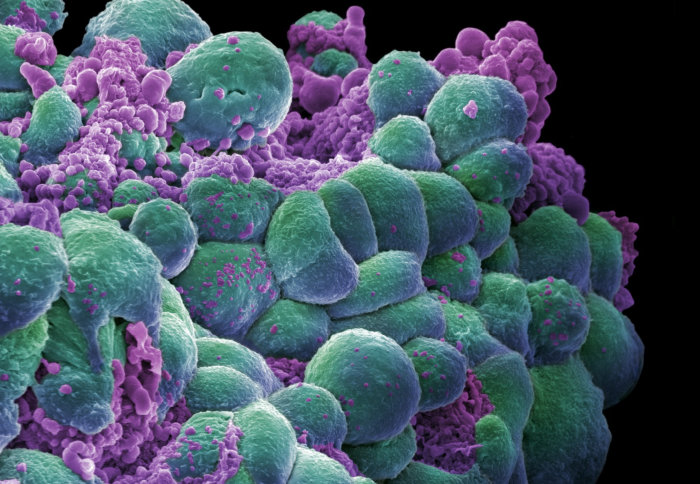
Lead image credit: 'Breast cancer cells' by Annie Cavanagh. Credit: Annie Cavanagh. CC BY-NC
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Genevieve Timmins
Academic Services