Supercharged natural killer cells may hold promise for cancer
by Kate Wighton
A type of ‘supercharged’ immune cell could be mass-produced to help fight cancer.
The researchers behind the early-stage finding, from Imperial College London, say the development could mark the next generation of cutting-edge immunotherapy treatments, called CAR-T therapies.
These personalised treatments involve reprogramming immune cells to kill cancer.
Cancer researchers and doctors are very excited about this therapy - it means that instead of talking to patients about a hospice, we can offer them a treatment that has a good chance of working Professor Anastasios Karadimitris Study author
NHS England announced on Friday it would be making the first ever CAR therapy licensed for the treatment of lymphoma available to patients on the Cancer Drugs Fund.
In the new study, funded by charity Bloodwise, the research team created a genetically engineered version of a cell called an invariant natural killer T-cell - CAR19-iNKT
Current CAR-T therapies are very expensive (around £300,000 per patient), and tend to be tailor-made for each patient. However, scientists behind the current study say their newer CAR-T therapy has the potential to be ten-fold cheaper, and can be mass-produced to enable one batch to be used on multiple patients.
The new research shows the CAR19-iNKT eliminated all cancer cells in 60 per cent of mice, with 90 per cent of animals surviving long-term.
The scientists behind the study, published in the journal Cancer Cell, are now considering human trials.
Army of cancer fighters
Professor Anastasios Karadimitris, senior author of the study from Imperial’s Department of Medicine, said: “These early findings suggest that a type of immune cell painstakingly engineered in the laboratory to be ‘supercharged’ holds promise as a new treatment for cancer patients.”
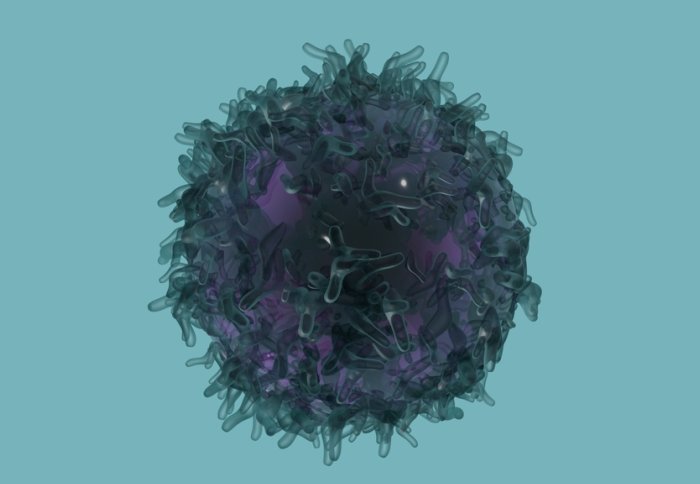
CAR (chimeric antigen receptor) therapy is a new type of immunotherapy that involves removing a type of immune cell from a patient’s blood, and genetically altering it in the laboratory. This creates a type of supercharged immune cell primed to seek and destroy cancer cells. This new, altered cell is then multiplied in the lab, and an army of these cancer-fighting cells are placed back into the patient.
This approach has been used to create new personalised treatment for leukemia and lymphoma, and resulted in up to one third of patients with no other therapeutic options going into long-term complete remission.
“Cancer researchers and doctors are very excited about this therapy - it means that instead of talking to patients about a hospice, we can offer them a treatment that has a good chance of working,” explained Professor Karadimitris who is based at Imperial’s Centre for Haematology.
Reprogramming cells
At the moment scientists use a type of immune cell called a T-cell to create CAR treatments called CAR-T.
However, in the new study, the Imperial scientists used a slightly different type of immune cell called iNKT .
Although these cells are much rarer in the body, the researchers found that CAR19-iNKT were more effective than CAR-T at eliminating cancer cells.
When the team used the genetically engineered cells to treat mice with lymphoma (a type of cancer of the lymph system) they found that 90 per cent of animals treated with CAR19-iNKT cells survived long term as compared to 60 per cent survival of mice treated with CAR-T cells.
The researchers were surprised to see the genetically engineered cells could travel to the brain, and also tackle large tumours – raising the possibility the technology could one day be used for brain tumours, as well as other cancers such as prostate and ovarian.
Life-saving treatments
Dr Alasdair Rankin, Director of Research at the blood cancer research charity Bloodwise, said: “Current CAR-T therapies being approved for use on the NHS are effective for a significant amount of patients, but not everyone responds to these treatments and they are extremely expensive to make.
Our animal experiments have shown the approach can eliminate cancer cells Dr Antonia Rotolo Study author
“This very promising research is in the early stages, but it paints an exciting picture of what the future of this treatment could look like. The possibility of cheaply mass-producing highly effective anti-cancer immune cells is in many ways the holy grail of CAR therapy. If successful, it would open up these life-saving treatments to many more patients.”
Dr Antonia Rotolo, first author of the study explained: “The current methods of producing CAR-T cells use the patient’s own T cells. However iNKT-cells can be sourced from healthy individuals, and unlike T cells don’t need to be matched to the patient. This means CAR19-iNKT cell treatment can be used off-the-shelf”
She added that the next step for the technology is to test it in patients: “Our animal experiments have shown the approach can eliminate cancer cells, but we cannot predict potential side effects - we can only investigate this through patient trials. This is an option we’re now exploring.”
The team are not yet recruiting for patients, but for further information on other clinical trials and patient support please visit Bloodwise.org.uk.
Imperial Innovations, the College's technology commercialisation partner, has patented the underlying cell processing technology and is working with Professor Karadimitris on commercial applications.
The study was also supported by the Imperial National Institute for Research Biomedical Research Centre, and Imperial Confidence in Concept.
-
‘Enhanced anti-lymphoma activity of CAR19-iNKT cells underpinned by dual CD19 and CD1d targeting’ by A. Rotolo et al is published in Cancer Cell
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division