Anti-inflammatory drug reduces key complication risk in HIV-positive TB patients
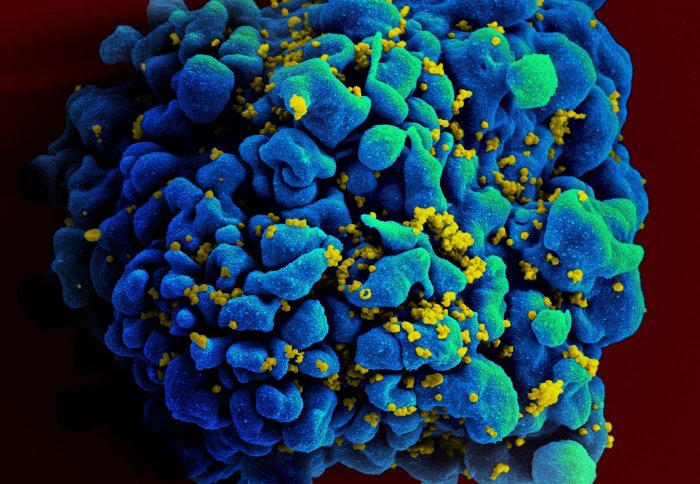
HIV-infected immune cell
Trial finds that prednisone can reduce the risk of TB-IRIS – a serious complication seen in HIV-positive tuberculosis (TB) patients.
A new study published in the New England Journal of Medicine shows that a four-week course of moderate dose prednisone – a medicine used to treat inflammation in the body – reduces the risk of TB-IRIS (tuberculosis-associated immune reconstitution inflammatory syndrome) by 30% in HIV-positive patients at high risk of developing the condition. The PredART trial is the first study to show that TB-IRIS can be prevented in these patients, and represents an important contribution to the body of knowledge on management of HIV-TB co-infection.
TB-IRIS is an excessive reaction by the immune system to TB infection, and is characterised by severe inflammation occurring shortly after initiation of antiretroviral therapy (ART) for HIV in patients who are also receiving tuberculosis treatment. TB-IRIS is a serious risk in people with HIV-associated TB, resulting in hospitalisation of a quarter of people who develop it.
“In patients with HIV, tuberculosis and very low CD4 counts, it is critical to start antiretrovirals within the first two weeks of treatment for tuberculosis, because this saves lives. But this also comes at the cost of a two-fold higher risk of developing a common inflammatory complication—TB-IRIS. Until now, no management strategy existed for preventing it. The findings of our study provide clinicians with a strategy for reducing the risk of this complication,” explains Professor Graeme Meintjes, PredART Principal Investigator.
The PredART trial was conducted by the Wellcome Centre for Infectious Diseases Research in Africa (CIDRI-Africa), a research group based at the University of Cape Town (UCT) which includes academics from Imperial College London, in collaboration with colleagues at the Institute of Tropical Medicine in Antwerp, Belgium. In the trial, researchers investigated whether providing people at high risk of TB-IRIS with moderate-dose prednisone could prevent development of the condition. The researchers enrolled HIV-positive patients who were initiating ART, had started tuberculosis treatment within 30 days before enrolment, and also had a very low number of CD4 cells (as HIV infection progresses, the number of these immunity-boosting cells in the body declines).
We now have first-rate evidence for a preventive strategy in selected patients Professor Robert Wilkinson Professor in Infectious Diseases
A total of 240 patients were enrolled, with 120 in each arm of the trial (prednisone or placebo). The researchers found that patients who received prednisone during the first four weeks of ART were less likely to develop TB-IRIS than those who received the placebo. Tuberculosis-associated IRIS was diagnosed in 56 patients in the placebo group and in 39 patients in the prednisone group, a reduction of 30%. Moderate dose prednisone was also found to be well tolerated by patients and there was no evidence of an increased risk of severe infections or cancers with this treatment.
Commenting on the significance of the findings, Imperial’s Professor Robert Wilkinson said: “TB-IRIS ironically arises as a consequence of two life-saving therapies. It is a common complication of combined treatments in Africa. We now have first-rate evidence for a preventive strategy in selected patients. A major opportunity is also presented by blood samples taken from the trial. In collaboration with Graeme Meintjes, Rachel Lai and I will be analysing these at Imperial to look for clues as to why the syndrome occurs, and also to predict more specific and effective treatments in future.”
‘Prednisone for the Prevention of Paradoxical Tuberculosis-Associated IRIS’ by Graeme Meintjes et al., is published in the New England Journal of Medicine.
This article was adapted from a press release by the Wellcome Centre for Infectious Diseases Research in Africa.
Image credit: NIAID via Wikimedia Commons
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Genevieve Timmins
Academic Services