Lack of key protein reduces brain connections in schizophrenia
by Ryan O'Hare
Lack of protein may lead to communication breakdown
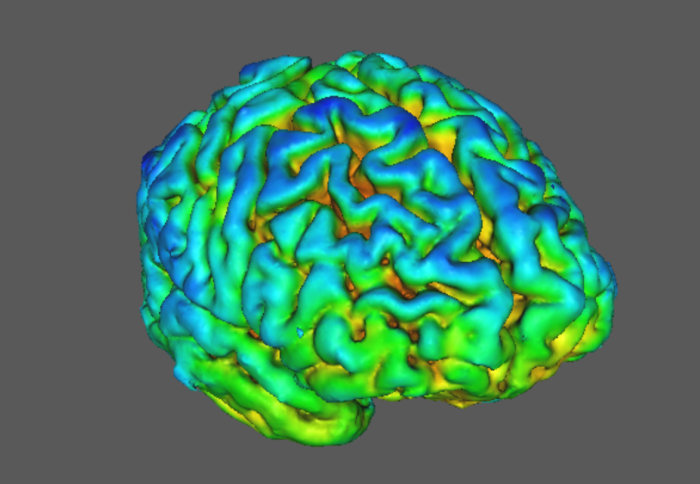
Brain scans have revealed for the first time how people with schizophrenia have reduced levels of a key protein which helps brain cells to communicate
The findings, published today in Nature Communications, have shown a lack of a protein called SV2A in the brains of those with schizophrenia, compared to those without.
According to the researchers who carried out the study, the findings suggest the protein could provide a new target for research into potential treatments.
Previous research had suggested that schizophrenia may be caused, in part, by problems in how brain cells communicate with one another. But scientists were only able to study this indirectly, using animal models or brain tissue from deceased patients.
Researchers from Imperial College London and King’s College London have used an advanced imaging technique called PET to detect these changes in living brains for the first time. The technique uses specially designed radioactive tracers, injected into the body, which can highlight the presence of key proteins.
In the latest study, the team scanned 18 adults with schizophrenia and compared them to 18 people without schizophrenia, using a tracer which binds to SV2A (synaptic vesicle glycoprotein 2A). Previous studies have shown the protein to be a good marker for the density of synaptic nerve endings in the brain.
Analysis revealed that levels of SV2A were lower in the front parts of the brain – regions of the brain involved in planning – in people with schizophrenia.
Potential new treatments
Professor Oliver Howes, who led the study, from Imperial’s MRC London Institute of Medical Sciences, and the Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said: “Our current treatments for schizophrenia only target one aspect of the disease – the psychotic symptoms – but the debilitating cognitive symptoms, such as loss of abilities to plan and remember, often cause much more long-term disability and there’s no treatment for them at the moment. Synaptic loss is thought to underlie these symptoms.
“Our lab at the MRC London Institute of Medical Sciences is one of the few places in the world with this new tracer, which means we’ve been able for the first time to show there are lower levels of a synaptic protein in people with schizophrenia. This suggests that loss of synapses could underlie the development of schizophrenia.
“We need to develop new treatments for schizophrenia. This protein SV2A could be a target for new treatments to restore synaptic function.”

Dr Ellis Onwordi, who conducted the research, from the MRC London Institute of Medical Sciences, Imperial College London, and the Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said: “Schizophrenia is a highly debilitating disorder, and the therapeutic options are too limited for many patients. To develop better treatments in the future we need studies like this to shine a light on how the extraordinarily complex wiring of the human brain is altered by this disease.”
“Having scans that can characterise the distribution of the approximately 100 trillion synapses in the living brain, and find differences in their distribution between people with and without schizophrenia, represents a significant advance in our ability to study schizophrenia.”
The people with schizophrenia who were scanned had all received antipsychotic medication, so the researchers wanted to exclude this as a factor in the synaptic dysfunction. They gave antipsychotic drugs, haloperidol and olanzapine, to rats for 28 days and found it had no effect on the levels of the protein SV2A.
Professor Howes said: “This is reassuring as it’s suggesting that our antipsychotic treatments aren’t leading to loss of brain connections.
“Next we hope to scan younger people in the very early stages to see how synaptic levels change during the development of the illness and whether these changes are established early on or develop over time.”
The researchers were funded by the Medical Research Council, part of UK Research and Innovation, and Wellcome. They were also supported by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
-
‘Synaptic density marker SV2A is reduced in schizophrenia patients and unaffected by antipsychotics in rats’ by Ellis Chika Onwordi et al. is published in Nature Communications.
This article is based on materials from the UKRI MRC.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ryan O'Hare
Communications Division