Medical students help tackle COVID-19 community health challenges
by Sarah Saxton
Third year medics have devised health interventions to help tackle some of the new challenges faced by GPs and their patients due to COVID-19.
The impact that COVID-19 is having on patients in the community has been a source of inspiration for third year MBBS students’ Community Action Projects (CAP). During their general practice placement, the students work with their GP tutor, local patients and communities to identify a problem that they think they can contribute to addressing over the course of their eight-week placement.
Course lead Dr Nina Dutta explained: “Due to COVID-19, this year’s GP placements have been very different - many of the patient consultations have been virtual and the practices have been running services differently. The pandemic has brought many challenges for GP practices and their patients, so I’m really pleased that through their Community Action Projects, our students have worked with local patients and communities to devise innovative solutions to some of these new problems.
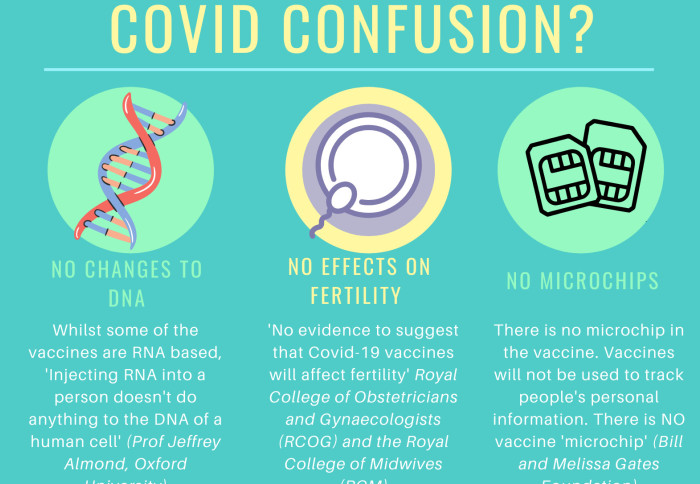
 “Several of the projects focused on the low levels of vaccine uptake amongst vulnerable patient groups and the students worked with local communities to explore the barriers and devise creative interventions to tackle this. They should be very proud that as a result of their work to tackle vaccine misinformation some patients had their concerns allayed and decided to have the vaccine.”
“Several of the projects focused on the low levels of vaccine uptake amongst vulnerable patient groups and the students worked with local communities to explore the barriers and devise creative interventions to tackle this. They should be very proud that as a result of their work to tackle vaccine misinformation some patients had their concerns allayed and decided to have the vaccine.”
Needs and assets analysis
Before kicking off their projects the students undertook a needs and assets analysis which involved desk research, drawing on local community information and talking to local patients and organisations such as Clinical Commissioning Groups, the local council and voluntary groups. This research enabled the students to refine and develop their project before they moved into the design and delivery phase.
Niamh Hardcastle and Emily Southall wanted to bring together information about local voluntary and community-based services that help tackle loneliness and social isolation in the elderly. Emily explained: “We contacted the community groups Age UK, Befriend London and Ealing Together who provide emotional support, friendship and practical support for elderly residents. These groups confirmed that a leaflet signposting to them would be beneficial, and the GPs we spoke to emphasised how useful if would be to have all the information about local services in one place.”
Phone calls, videos and leaflets
Once the students had agreed on their health intervention, they had to decide how to best reach their target audience to help achieve their objectives.
Hasan Rahij explained his group’s approach: ‘We felt the best way to tackle vaccine hesitancy was to make two short videos (one in English, one in Hindi) addressing some of the common myths and concerns regarding the COVID-19 vaccine. Posters and leaflets in healthcare settings can often be ignored by patients, especially during COVID when they are stuck at home. But an informative video that can be viewed on a phone or tablet, is a lot more accessible and effective.”
For other groups, speaking directly to patients was central to their project. Archit Singhal explained why his group adopted this approach: “We rang patients to help us understand their reasons for vaccine refusal. This allowed us to tailor the contents of an information leaflet on the vaccine to the concerns of the local community. The aim of the leaflet was to inform administrative staff thus facilitating more effective conversations with patients and ultimately leading to an increased uptake in the vaccine.”
Severe asthma and COVID-19
Marion Jenkyns and Jack Tighe worked on a project to help asthmatic patients understand if their asthma was defined as ‘severe’.  Those with severe asthma would be prioritised for the COVID-19 vaccine whilst others would receive it with their age group as they were at no greater risk than the general population. Whilst this should be a relatively simple thing to determine, patients often had queries.
Those with severe asthma would be prioritised for the COVID-19 vaccine whilst others would receive it with their age group as they were at no greater risk than the general population. Whilst this should be a relatively simple thing to determine, patients often had queries.
Marion and Jack focused their CAP on finding information to address these queries and presenting it in an informative and easy to understand way. Their simple infographic asked patients a series of ‘yes or no’ questions. Their answers helped patients to determine if their asthma was defined as severe and therefore if they would be called for a vaccine in one of the priority groups.
The infographic was sent to 175 patients with asthma aged 18-50 via the GP practice’s text system. Jack said: “I was really impressed to see how useful our infographic was to patients, we had found it so frustrating getting all this information together so to get it across so well was a really proud moment.”
Evaluation and sustainability
Evaluation is a central component of all CAPs. Students are encouraged to consider what went well as well as thinking about what changes they might make if they were to do it again or had more time to develop it.
With GP practices experiencing significant demands on their time, devising CAPs that are sustainable is vital. Marion explained: “When we had almost completed the project, articles about confusion that patients with asthma had over vaccine priority hit the news. We realised that we had picked up on a real issue, and that our intervention could have a really significant impact not only in our practice, but on a much greater scale.” The asthma infographic resulted in a reduced volume of calls from patients to their placement practice and was subsequently sent to all COVID-19 leads in Ealing.
Find out more
Students studying for an undergraduate medical degree (MBBS) at Imperial have direct contact with patients in primary and secondary care from the start of their degree and they also receive a BSc qualification. During their primary care courses, all students have the opportunity to work with local patients and communities on impactful quality improvement projects such as the Year 3 Community Action Project, making a meaningful difference while learning.
For further information, please contact Dr Arti Maini, Deputy Director for Undergraduate Primary Care Education and a Theme Lead for Medical Education Innovation and Research Centre (MEdIC) a.maini@imperial.ac.uk
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Sarah Saxton
Communications Division