Key enzyme aggravates colorectal cancer in obese patients
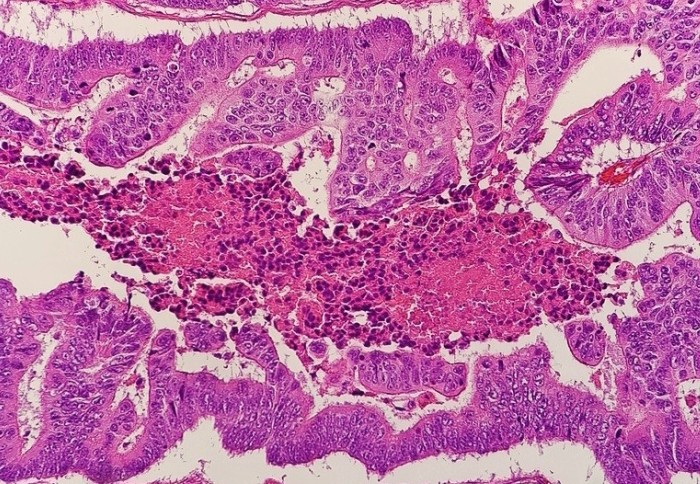
Micrograph of colorectal carcinoma
New research suggests the enzyme CES1 helps tumour cells to survive and drives aggressive colorectal cancer in obese patients.
Colorectal cancer, or colorectal carcinoma (CRC), occurs when abnormal cells start to divide and grow in an uncontrolled way in the large bowel (colon) or back passage (rectum).
Globally, 1.8 million people are diagnosed with CRC each year. It is also the second most common cause of cancer death in the UK, accounting for 10% of all cancer deaths.
Worldwide obesity has tripled since 1975 and more than 1.9 billion adults are overweight. Obesity is a major risk factor for CRC, increasing both disease recurrence and mortality rates in patients. However, while previous research has shed light on the molecular mechanisms which underlie increased incidence in obese people, precisely how obesity drives the more aggressive clinical behaviour of CRC is poorly understood.
Now, a team of researchers from Imperial College London have published findings in the Journal of Clinical Investigation, which shed new light on this question.
Crossed signals
Previous research has shown that a specific signalling pathway in our cells, known as the NF-κB pathway, plays an important role in the development of certain cancers and inflammatory conditions. Normally, the NF-κB pathway helps to regulate our immune system’s response to infection. However, when it goes awry, NF-κB can trigger cells to replicate uncontrollably, causing tumours to develop and spread more rapidly.
In past studies, the pathway has been shown to drive tumour-promoting inflammation and cancer cell survival in CRC. However, NF-κB’s effect on the metabolic adaptations that fuel aggressive disease in CRC patients had not been established.
Now, the current study suggests that the pathway drives the expression of an enzyme called CES1, which in turn promotes aggressive CRC.
Adding fuel to the fire
Tumours generally contain a lower amount of vital nutrients, such as sugars, than normal tissues due to their abnormal and inefficient blood supply and the increased energy consumption by rapidly dividing tumour cells. This poses a significant challenge for tumour cells which, if not met, causes them to starve and eventually die. The findings from the current study suggest that fat tissue in obese people helps tumours to get around this problem in several different ways.
Firstly, the researchers found that fat increases local inflammation, which in turn helps tumours to produce enzymes including CES1, which cleaves fats normally stored within tumour cells. The products of this reaction are then used as a source of energy to feed tumour cells in an environment that is typically low in sugars.
Owing to its unique biological properties, fat initiates a cascade of events within tumour cells, enabling them to become more resilient to stress and more mobile. This allows them to spread to other parts of the body, where they are more fit to survive and grow, forming so-called metastases, which are by far the most common cause of death in cancer patients.
Finally, being obese or overweight means there is an increase in the overall supply of fat that tumour cells can use as a source of energy.
However, while CES1 may help tumours to survive and grow, it also makes them more vulnerable to treatment with new drugs.
Based on data gathered in the lab and animal models, the team behind the study have also shown that blocking CES1 impairs the ability of tumour cells to adapt to and survive in low-sugar environments. Importantly, because blocking CES1 appears to have no significant toxic adverse effects in normal cells, this approach may lead to the development of safer and more effective treatments for currently hard-to-treat forms of CRC in obese patients.
Next steps
Commenting on the significance of the paper, lead author Professor Guido Franzoso, based at Imperial's Department of Immunology and Inflammation, said: “The findings provide a molecular mechanism for the more aggressive behaviour of CRC in obese individuals by uncovering a previously unknown linkage between NF-κB signalling and tumour-based inflammation with obesity, fat metabolism and aggressive tumour biology in metastasis-prone mesenchymal colorectal tumours.”
“We also identify CES1 as a druggable therapeutic target in hard-to-treat subtypes of CRC which generally do not respond to conventional immune checkpoint immunotherapy.”
The study team will now look to prove the efficacy of their new therapeutic approach in CRC patients by conducting further tests in tumour tissue obtained from clinical settings.
First author Dr Daria Capece noted: “We also need to develop better compounds that one day we hope can be used in the clinic to improve the treatment of CRC patients who are obese”.
Co-author and colorectal surgeon Dr James Kinross said: “The obesity pandemic is changing the biology of colorectal cancer. Obese patients are 30% more likely to suffer this disease, and their cancer treatment outcomes are much worse than the general population.
"This data is important as it will allow us to better stratify treatment for colorectal cancer in this high-risk group of patients. This exciting new therapeutic target means we can also improve cancer outcomes and potentially even prevent this devastating disease”.
‘Enhanced triacylglycerol catabolism by Carboxylesterase 1 promotes aggressive colorectal carcinoma’ by Daria Capece, Daniel D'Andrea et al. is published in The Journal of Clinical Investigation
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Genevieve Timmins
Academic Services