Microbiome signature for ischaemic heart disease unravelled
New international studies have characterised the imbalanced gut bacteria of patients with myocardial infarction, angina and heart failure.
Two papers published in Nature Medicine, from the MetaCardis consortium, co-led by Imperial's Professor Marc-Emmanuel Dumas, show how major disturbances occur in the gut microbiome of patients suffering from heart disease.
The team of scientists and institutions from the UK, France, Denmark, Germany, Sweden and Israel have unravelled a microbiome signature for ischaemic heart disease (IHD), previously known as coronary artery disease, after carefully unpicking the contribution from medication and risk factors such as age, sex, country, and metabolic conditions such as diabetes and obesity
Professor Marc-Emmanuel Dumas, jointly based in the Department of Metabolism, Digestion and Reproduction and National Heart and Lung Institute, explains: "By combining a study design that mirrors the natural history of cardiometabolic diseases and state-of-the-art technologies such as metabolomics, shotgun metagenomics, and machine learning, we identified a series of escalations from metabolic health to dysmetabolism and eventually culminating with IHD, which were not reducible to geographical variation, age, sex, or medication."
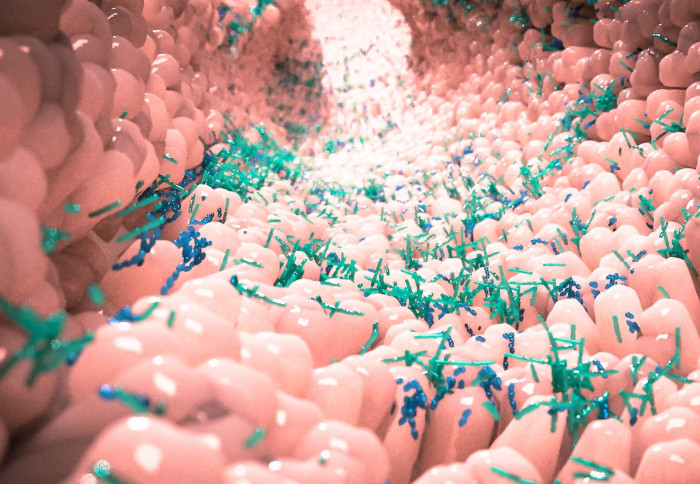
The gut microbiome
The human gut contains trillions of bacteria, collectively called the gut microbiome, which may have positive and negative effects on human health. When in balance they function as an inner chemistry factory producing numerous compounds that promote good health. However, an unhealthy lifestyle -- poor diet, smoking, lack of physical activity or disease -- can disrupt the balance, leading the microbiome to instead produce compounds that may trigger multiple non-communicable chronic disorders in people at high genetic risk, including ischaemic heart disease.
Scientists have already discovered that the gut microbiome is altered in people with chronic heart disease and they have subsequently identified compounds that are produced by the diseased microbiome, for instance, a bacterial compound called trimethylamine (TMA) that after modification in the liver of the human host causes arteriosclerosis.
However, these findings of the altered gut microbiome are challenged because they were achieved in studies of medicated patients. Patients with heart disease are given several different drugs, each of which is known to modify the gut microbiome. As a result, it was unclear whether drugs or heart disease itself caused the disrupted gut microbiome of people with cardiovascular disorders.
A further complication lies in the fact that heart disease often develops alongside the early stages of overweight and type 2 diabetes, which are also characterized by having disrupted gut microbiomes. As a result, it remained to be shown whether an imbalanced gut microbiome is a feature of heart disease itself.
Heart diseases cause major disturbances in the gut microbiome
To answer these critical questions a European consortium of researchers established the EU-funded MetaCardis research project in 2012 to investigate the role of gut microbes in cardiometabolic disease.
Speaking about the study structure, Professor Oluf Pedersen, co-lead researchers from the University of Copenhagen, said: “We applied a study design that mirrors heart disease initiation and escalation over time, substituting for a longitudinal study of the gut microbiome that otherwise would be impossible to perform given the 50-60 years it takes to develop symptoms of arteriosclerosis and have the diagnosis of heart disease,”
Researchers recruited 1,241 middle-aged people from Denmark, France and Germany including healthy individuals, individuals with obesity and type 2 diabetes but lacking a diagnosis of heart disease, and patients with either myocardial infarction, angina pectoris or heart failure. The investigators quantified about 700 different bacterial species and estimated their functions in the gut microbiome and compared these findings to more than 1,000 compounds circulating in blood with many of these compounds originating from the inner gut chemistry factory.
“We found that about half of these gut bacteria and blood compounds were modified by drug treatment and not directly related to heart disease or the early disease stages like diabetes or obesity occurring prior to diagnosis of heart disease,” Prof Pedersen continued. “Among the remaining half, about 75 percent of the disturbances of the gut microbiome occurred in the early disease stages of overweight and type 2 diabetes, many years before patients noticed any symptoms of heart disease.”
The findings of gut microbiome and blood compound changes in patients with one of the three heart disorders, acute myocardial infarction, were validated and extended in a study from Israel that is reported in the same issue of Nature Medicine.
Next steps
This study potentially paves the way to use a person’s microbiome to evaluate their individual risk of developing dysmetabolism and IHD. The team is now working on a series of tests for microbiome markers, targeting cardiometabolic health, which will be able to point a patient to the right treatment based on their microbiome makeup and products.
Prof. Dumas also discussed the possibility of reducing IHD risk by improving microbiome health: "It is entirely possible to harness microbiomes through a range of interventions and diets. For instance, increasing your intake of beneficial nutrients (prebiotics), supplementing beneficial bugs (probiotics and live biotherapeutics), or innovative treatments based on compounds made by the microbiome (postbiotics).
"So yes, feeding your microbiome to improve cardiometabolic health is one possible outcome of these findings. But also the ability to 'learn from nature' to develop new treatments is also an intriguing possibility."
However, Prof. Dumas also highlights that "although these clinical studies represent an important milestone in the cardiometabolic microbiome field, they remain observational and it is crucial to invest in longitudinal studies to monitor long-term trends and clinical trials focussing on actionable microbiome targets such as individual microbes or microbial consortia and their metabolic products."
Main image credit: Shutterstock.
For any press inquiries, please contact Ryan O'Hare.
Some content for this article was provided by the University of Copenhagen - The Faculty of Health and Medical Sciences.
Microbiome and metabolome features of the cardiometabolic disease spectrum. Sebastien Fromentin, Sofia K. Forslund, Kanta Chechi, Judith Aron-Wisnewsky, Rima Chakaroun, Trine Nielsen, Valentina Tremaroli, Boyang Ji, Edi Prifti, Antonis Myridakis, Julien Chilloux, Petros Andrikopoulos, Yong Fan, Michael T. Olanipekun, Renato Alves, Solia Adiouch, Noam Bar, Yeela Talmor-Barkan, Eugeni Belda, Robert Caesar, Luis Pedro Coelho, Gwen Falony, Soraya Fellahi, Pilar Galan, Nathalie Galleron, Gerard Helft, Lesley Hoyles, Richard Isnard, Emmanuelle Le Chatelier, Hanna Julienne, Lisa Olsson, Helle Krogh Pedersen, Nicolas Pons, Benoit Quinquis, Christine Rouault, Hugo Roume, Joe-Elie Salem, Thomas S. B. Schmidt, Sara Vieira-Silva, Peishun Li, Maria Zimmermann-Kogadeeva, Christian Lewinter, Nadja B. Søndertoft, Tue H. Hansen, Dominique Gauguier, Jens Peter Gøtze, Lars Køber, Ran Kornowski, Henrik Vestergaard, Torben Hansen, Jean-Daniel Zucker, Serge Hercberg, Ivica Letunic, Fredrik Bäckhed, Jean-Michel Oppert, Jens Nielsen, Jeroen Raes, Peer Bork, Michael Stumvoll, Eran Segal, Karine Clément, Marc-Emmanuel Dumas, S. Dusko Ehrlich, Oluf Pedersen. Nature Medicine, 2022; DOI: 10.1038/s41591-022-01688-4
Metabolomic and microbiome profiling reveals personalized risk factors for coronary artery disease. Yeela Talmor-Barkan, Noam Bar, Aviv A. Shaul, Nir Shahaf, Anastasia Godneva, Yuval Bussi, Maya Lotan-Pompan, Adina Weinberger, Alon Shechter, Chava Chezar-Azerrad, Ziad Arow, Yoav Hammer, Kanta Chechi, Sofia K. Forslund, Sebastien Fromentin, Marc-Emmanuel Dumas, S. Dusko Ehrlich, Oluf Pedersen, Ran Kornowski, Eran Segal. Nature Medicine, 2022; DOI: 10.1038/s41591-022-01686-6
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Benjie Coleman
Department of Surgery & Cancer