'Silent’ mutations help bacteria to evade antibiotics
Researchers have discovered a new way hospital-acquired infections resist antibiotics, through a ‘silent’ genetic mutation.
Bacteria can acquire resistance to antibiotics through random mutations in their DNA that provide them with an advantage that helps them survive. Finding genetic mutations, and discovering how they help bacteria to survive antibiotic attack, is key to helping us fight back with new drugs.
The researchers have now discovered a ‘silent’ mutation in the genetic code that leads to antibiotic resistance. Typically, mutations of this kind would be overlooked, and they may already be present in other infectious bacteria.
The team, led by researchers at Imperial College London and including international collaborators, published their results today in the journal Proceedings of the National Academy of Sciences.
Rising resistance
The researchers looked at the bacterium Klebsiella pneumoniae, which causes infections in the lungs, blood and wounds of those in hospitals, with patients that have compromised immune systems, such as those in intensive care units, being especially vulnerable.
This discovery should change how we view the genetic code in bacteria and potentially indicates that we in the scientific community have overlooked other similar mutations that may have important effects. Dr Joshua Wong
Like many bacteria, K. pneumoniae are becoming increasingly resistant to antibiotics, particularly a family of drugs called carbapenems. These important drugs of last resort are used in hospitals when other antibiotics have already failed.
As rising resistance to carbapenems could dramatically affect our ability to treat infections, carbapenem-resistant K. pneumoniae are classified as ‘critical’ World Health Organization Priority 1 organisms.
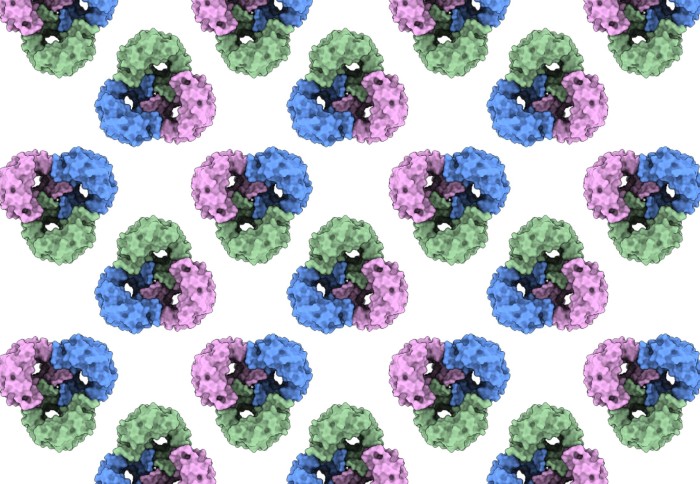
In order to be effective, antibiotics need to get inside bacteria, and in K. pneumoniae this happens via a channel in the bacterium’s outer membrane, formed by a protein called OmpK36. The team discovered a genetic mutation that makes the bacteria produce less of the protein, effectively shutting some of these channels and keeping carbapenem antibiotics out.
‘Silent’ mutations
This mutation, however, works differently to standard mutations that result in antibiotic resistance. Usually, mutations change the genetic code so that when it is ‘read’ by ribosomes and converted into a protein, it produces a different chain of amino acids with different functions.
This mutation still produces the same amino acid chain, but alters the structure of an important mRNA intermediate, preventing ribosomes reading the code and producing protein from it.
When looking for mutations, genomic techniques are usually searching for changes to the amino acid sequence. However, since this mutation alters a structure, rather than the sequence itself, it could be thought of as a ‘silent’ mutation.
First author Dr Joshua Wong, from the Department of Life Sciences at Imperial, said: “In the age of big data and genomics, mutations such as we have discovered may be considered ‘silent’ as the genetic code results in the same protein sequence.
“This discovery should change how we view the genetic code in bacteria and potentially indicates that we in the scientific community have overlooked other similar mutations that may have important effects. Our work focuses on a single mutation but fundamentally changes how we interpret mutations, especially those that were thought to be silent.”
Driven by antibiotic use
The team at Imperial, who characterised the mutation, worked with teams at the University of Oxford, the University of Florence, and Harvard University to identify the distribution of the mutation globally, assess resistance levels, and to determine how the mutation affected the intermediate mRNA structure.
Using data from resistant bacteria samples collected globally, the team showed that the mutation had arisen several times independently. This suggests it is not random, and is instead driven by the need of the bacteria to defend itself again the antibiotics.
Lead researcher Professor Gad Frankel, from the Department of Life Sciences at Imperial, said: “The mutation evolved on several occasions independently, and this tells us that this novel mechanism is not a one-off fluke, but instead driven by antibiotic consumption. This suggests that the mutation occurs under antibiotic pressure and highlights the side effects of excessive antibiotic usage in hospitals and other settings.”
The team now hope their finding will be incorporated into bioinformatic tools that analyse genetic sequences to identify the presence of the mutation, as was done with a previous mechanism the team discovered.
They will also continue to work with their collaborators to look for other important mutations in this key pathogen.
-
‘Recurrent emergence of Klebsiella pneumoniae carbapenem resistance mediated by an inhibitory ompK36 mRNA secondary structure’ by Joshua L. C. Wong et al. is published in Proceedings of the National Academy of Sciences.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Hayley Dunning
Communications Division