Study reveals extent of lung scarring after COVID hospitalisation
by Ellyw Evans
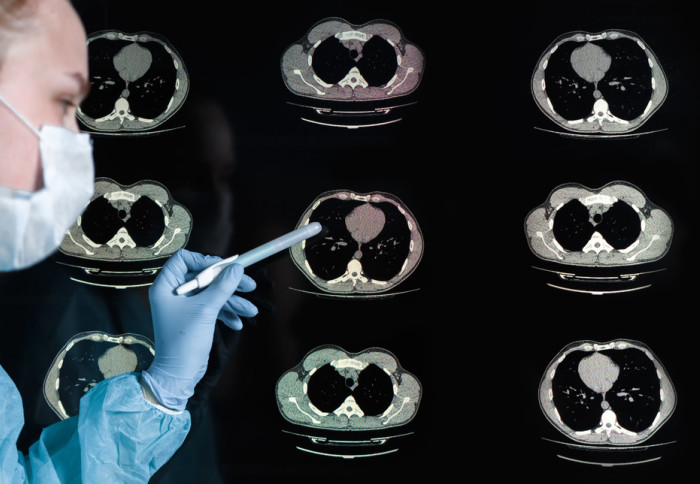
Research led by Imperial estimates that 11% of hospitalised COVID-19 patients had lung scarring after recovery from the illness.
A new study of 209 people discharged from hospital following COVID-19 admission has estimated the percentage who had a type of fibrotic lung damage. This type of lung damage is characterised by lung scarring and requires ongoing follow-up care.
The interim analysis of the UK Interstitial Lung Disease (UKILD) Post COVID study is published in the American Journal of Respiratory and Critical Care Medicine.
This work represents a huge effort to collect post-discharge data from thousands of COVID patients nationwide Prof Gisli Jenkins
The research, which is led by the UKILD consortium in partnership with the PHOSP-COVID consortium, offers the largest assessment of the prevalence of abnormal lung patterns in patients hospitalised for COVID-19 to date.
The study team, involving Imperial researchers, applied the characteristics of the 209 study participants who had CT scans to a wider post-hospitalisation cohort of almost 3,500 people without a CT to stratify the risk of residual lung abnormalities.
Abnormal lung patterns
Dr Iain Stewart, lead author who is an Advanced Research Fellow at Imperial's Margaret Turner Warwick Centre for Fibrosing Lung Disease, said: "We estimated that up to 11% of hospitalised COVID-19 patients had fibrotic patterning after recovery from the acute illness. Whilst many people experience prolonged breathlessness, the major implication of these findings is that a substantial number of people discharged from a COVID-19 hospitalisation may also have fibrotic abnormalities in their lungs.”
The study team highlight that these results should help concentrate efforts to closely follow at-risk patients. This follow-up should include repeat radiological imaging and lung function testing.
“For some people, these fibrotic patterns may be stable or resolve over time, while for others they may lead to longer term lung fibrosis progression, worse quality of life and decreased life expectancy. Earlier detection of progression is essential to improving outcomes,” added Dr Stewart.
UK-wide collaboration
The study was performed in co-operation with the PHOSP (post hospitalisation)-COVID study, which consists of researchers and clinicians from across the UK, to look at how different patients who were hospitalised with COVID-19 subsequently recovered. The researchers identified patients with thoracic CTs from the PHOSP-COVID database. The study excluded patients in PHOSP-COVID who had interstitial lung disease prior to COVID-related hospital admission.
Professor Gisli Jenkins, study author and Margaret Turner Warwick Chair of Thoracic Medicine, said: “This work represents a huge effort to collect post-discharge data from thousands of COVID patients by clinical teams nationwide, and reflects a strong collaborative approach between the PHOSP study investigators and the UKILD consortium. We are enormously grateful to all the patients and partners involved, including funding from the UKRI.”
The next phase of the study is a primary analysis, which will be performed at 12 months. At that time, the study team will also use linked electronic health records of hospital admissions and mortality data to support the analyses. Final results are expected in early 2023.
'Residual lung abnormalities following COVID-19 hospitalisation: interim analysis of the UKILD Post-COVID study' by Iain Stewart et al is published in American Journal of Respiratory and Critical Care Medicine.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ellyw Evans
Faculty of Medicine Centre