Shape-shifting cancer cell discovery reveals potential skin cancer drug targets
A new technique allows scientists to see cells in 3D, and determine how different genes affect the shapes they adopt.
Cancer cells can change shape to travel around the body and spread (metastasise), but how they know when to do this has remained elusive.
In the future, we hope that the approach demonstrated here can be applied to address a wide range of questions in cancer biology. Professor Chris Dunsby
Researchers have now used a new technique to identify two genes that control how melanoma skin cancer cells change shape in response to their environment – offering two potential drug targets to stop the cancer spreading.
Cancer cells can change shape to move around the body, becoming drill-shaped to ‘poke’ through dense tissue like bone, or round and squishy to squeeze through soft tissues and get into the blood.
In a study published in Cell Reports, scientists at The Institute of Cancer Research, London, and Imperial College London have uncovered genes affecting how cells know what environment they are in and therefore which shape to choose.
Professor Chris Bakal, Professor of Cancer Morphodynamics at The Institute of Cancer Research, London, said: “Once cancer becomes metastatic and spreads to different parts of the body, it can be quite difficult to treat.
“This research has given us insight into the tricks that cancer cells are using to keep growing and spreading. We’ve identified two genes which could, in the future, be targeted to stop melanoma cancer from changing shape and metastasising.”
3D view
The team developed a new system to study cells in 3D environments – mimicking different parts of the body. Until now, most research has studied cells on hard 2D plastic surfaces.
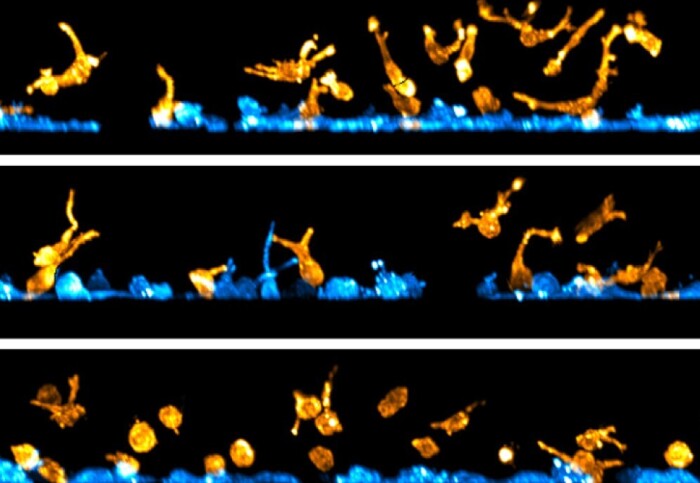
A unique microscope called stage-scanning oblique plane microscopy (ssOPM) was used to take 3D images of melanoma cells – either stuck to a flat and rigid surface or embedded within a 3D soft collagen hydrogel.
By analysing the 3D images taken of 60,000 cells when certain genes were ‘switched off’, the researchers identified two genes that are important for melanoma cells to change their shape in response to their environment.
The researchers believe these genes, TIAM2 and FARP1, could be targeted to prevent melanoma cancer from metastasising. These genes are good candidates for drug discovery as they have a structure similar to other proteins for which drugs are already in pre-clinical development.
Questions in cancer biology
Professor Chris Dunsby, from the Department of Physics at Imperial College London, said: “This study is the first to apply a new high-content microscopy technique called oblique plane microscopy to study many thousands of cells in 3D. In the future, we hope that the approach demonstrated here can be applied to address a wide range of questions in cancer biology.”
The research team are currently creating AI-based technologies to make predictions about which drugs might be successful, by using these 3D images of cells – which could reduce the time taken to develop new drugs.
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London, said: “By using an innovative technique to study cells as if they were in a human, rather than in a laboratory, our scientists have uncovered a mechanism which cancer cells are using to move around the body.
"We know that most cancer deaths occur because cancer has spread from the original tumour to other parts of the body. I hope that further research will lead to the development of new treatments for metastatic melanoma.”
-
This research was funded by The Institute of Cancer Research (ICR) itself, which is both a research institute and a charity, together with Cancer Research UK, Imperial College London, and The Engineering and Physical Sciences Research Council.
‘Environmentally dependent and independent control of 3D cell shape’ by Lucas G. Dent et all is published in Cell Reports.
Based on a press release by The Institute of Cancer Research.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Hayley Dunning
Communications Division