Map of blood vessel cells could transform treatments of vascular diseases
The research offers new insights into the diversity and specialisation of vascular cells, which could inform targeted treatments for vascular disease.
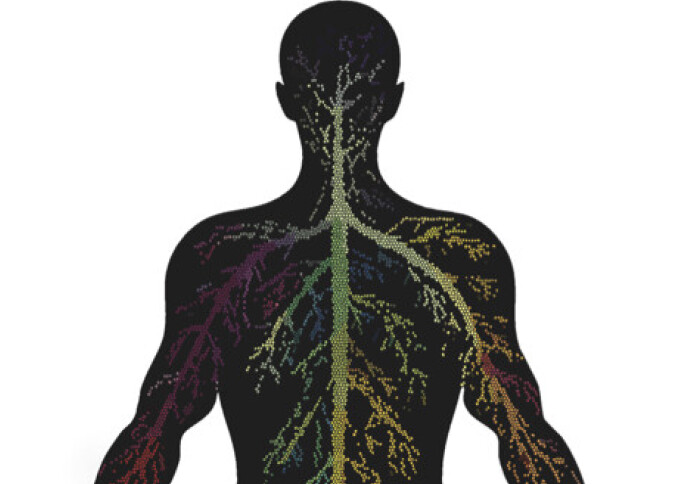
A pioneering study, co-led by the National Heart and Lung Institute (NHLI) at Imperial and the Cambridge Stem Cell Institute, has mapped the molecular diversity of human blood vessel cells, revealing how these cells vary across different organs and blood vessel types.
Published in Nature Medicine, the study charted over 67,000 vascular cells across 19 organs to create a high-resolution map, using a cutting-edge technique called single cell transcriptomics, which identifies active genes at a single-cell level. This approach allowed the team to capture unique molecular ‘states’ that correspond to specific cell functions and characteristics, providing insights that could help to improve treatments for cardiovascular disease, and diseases with vascular involvement, such as cancer, diabetes, and hypertension.
“Previously to this, we didn’t know the extent to which vascular cells and their molecular signatures varied across the human body. Sam Barnett Co-lead author
Co-first author Sam Barnett, PhD student at the NHLI, said, “Previously to this, we didn’t know the extent to which vascular cells and their molecular signatures varied across the human body. Now, we have a more complete understanding of the molecular and cellular architecture of vessels, and that could allow the creation of drugs that precisely target specific vascular cells in diseased organs and tissues.
For example, if scientists want to make a drug that targets blood vessels in the brain, they can now distinguish those cells from other organs’ vessels, enabling them to produce a medication that only affects the intended ones and reduces unwanted side-effects.”
Understanding the hidden diversity of blood vessels
Blood vessels span nearly 100,000 km in the human body, performing essential functions such as delivering oxygen, regulating blood pressure, and supporting immune responses. Despite their importance, the unique molecular makeup of blood vessel cells across different organs had not been well understood – until now.
Existing studies have primarily focused on the differences between blood vessels within specific organs. However, this new research highlights two main types of diversity within and across organs – angiotypic diversity, which refers to differences between arteries, veins, and capillaries, and organ-specific diversity, whereby certain organs contain specialised vascular cells, which are adapted to meet the functional needs of each organ.
For example, endothelial cells in the spleen help filter damaged red blood cells, while blood-brain barrier cells prevent harmful substances from entering the brain.
In total, the researchers identified 42 distinct vascular cell types, each with specific molecular ‘signatures’ that reflect the structural and functional demands of the tissue they support. For example, large arteries require stronger structural support for blood flow, while small capillaries are specialised for efficient oxygen and nutrient exchange and organ-specific functions.
"This atlas of healthy blood vessel cells represents a fundamental reference to understand the changes occurring in blood vessels in a wide range of diseases" Michela Noseda Co-lead author
Dr Michela Noseda, Reader in Cardiovascular Science at the NHLI and a co-lead author of the study said, “Blood vessels are involved in the progression of most diseases. This atlas of healthy blood vessel cells represents a fundamental reference to understand the changes occurring in blood vessels in a wide range of diseases, such as hypertension, diabetes, cancer and heart disease.”
Understanding how blood vessels communicate
Blood vessel cells work in harmony with each other and with nearby tissue cells. The authors mapped several communication pathways, or molecular ‘conversations’ that help blood vessels work together, such as by helping to coordinate functions like cell growth and immune response. Understanding these pathways in detail provides insights into how blood vessels maintain tissue health and how disruptions in these pathways might lead to disease.
Working towards targeted therapies for vascular diseases
The research is part of the international Human Cell Atlas (HCA) initiative, which is creating comprehensive reference maps of all human cells as a basis for both understanding human health and diagnosing, monitoring and treating disease. As an open, scientist-led consortium, HCA is a collaborative effort of researchers, institutes and funders worldwide, and will provide a foundation to transform and democratise global healthcare.
The study paper is one of a set of 40 publications in Nature Portfolio journals released today, representing a milestone leap in scientific understanding of the human body.
Professor Sarah Teichmann from the Cambridge Stem Cell Institute, said, “It is an exciting time in the Human Cell Atlas project, where we are at a stage of integrating suspension cell and nuclear RNA sequencing data with deep learning methods, revealing new insights into cell types and cell states. These reference data sets will serve the community as we enter the next stage of the Human Cell Atlas project, advancing our coverage of the human body in the era of spatial genomics.”
The study opens up new opportunities for further investigation, including understanding how vascular cells differ with age, sex and ancestry. The map also serves as a reference for identifying active genes that could be targeted to treat diseases like cancer, diabetes, and inflammatory conditions more precisely, without impacting healthy tissues. Additionally, insights into cell communication pathways may lead to therapies that promote blood vessel healing, critical for treating wounds, heart attacks, and strokes.
The study was funded by the Wellcome Trust, the EU’s Horizon 2020 Framework Programme, the British Heart Foundation, the Takeda Science Foundation and Rosetrees Trust, and was supported by the NHLI, NIHR Imperial Biomedical Research Centre and the British Heart Foundation Centre for Research Excellence at Imperial College London, as well as by the British Society for Heart Failure and EMBO Postdoctoral Fellowship.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Emily Medcalf
National Heart & Lung Institute