Meet the Imperial experts fighting bacterial resistance through innovation
by Meesha Patel, Lou Lee
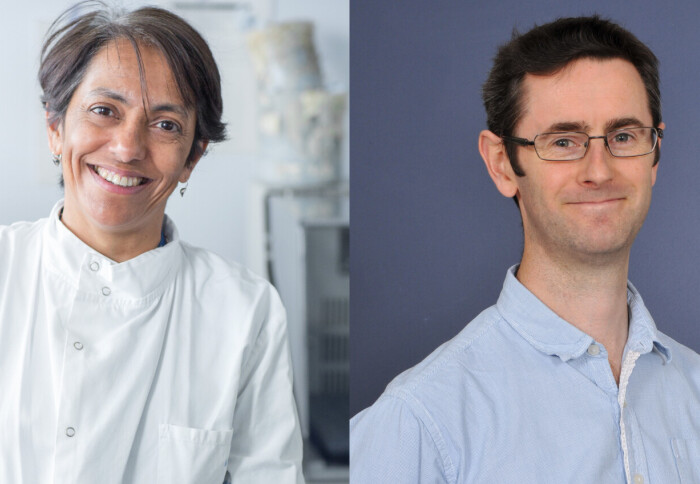
Professor Shiranee Sriskandan and Dr Andrew Edwards shed light on the vital work of Imperial’s Centre for Bacterial Resistance Biology (CBRB).
To mark World Antimicrobial Resistance (AMR) Week, Professor Shiranee Sriskandan and Dr Andrew Edwards shed light on the vital work of Imperial’s Centre for Bacterial Resistance Biology (CBRB) in tackling AMR. They explain how resistance arises, and discuss the pioneering strategies being used to combat this global health challenge.
Formerly known as the MRC Centre for Molecular Bacteriology and Infection, the Centre for Bacterial Resistance Biology has been bringing together medical scientists, biologists, and clinicians to better understand bacterial infection and immunity for over two decades.
The Centre is jointly hosted by the Departments of Infectious Disease and Life Sciences, and is led by co-directors Professor Mariagrazia Pizza and Professor Shiranee Sriskandan.
Tell me a bit about who you are and what you do at Imperial.
Professor Shiranee Sriskandan: I’m a clinical infectious diseases academic so I look after patients with infections in hospital as well as conducting research in this area in the university. My main research focus is on Group A streptococcal infections, which can cause many different types of infections that range from minor to serious, from strep throat to toxic shock. I’m also Co-Director of the Imperial Centre for Bacterial Resistance Biology (CBRB) .
Dr Andrew Edwards: I’m a Reader in Molecular Microbiology in the CBRB. My research focuses on understanding how antibiotics work, why they sometimes fail, and how we can address those failures – whether through developing new drugs or using combinations of existing ones.
How does antimicrobial resistance arise?
Dr Andrew Edwards: Antibiotics have revolutionised medicine, enabling treatments for everything from minor infections to cancer therapy and organ transplants. They work by stopping bacterial growth, allowing the immune system to clear the infection. However, resistance arises when bacteria either acquire resistance genes from other bacteria or mutate in ways that stop antibiotics from working – for instance, by changing the structure of proteins antibiotics target. Most antibiotics are derived from natural sources, meaning bacteria have evolved resistance mechanisms over millennia. The widespread use of antibiotics since the 1930s has accelerated the spread of these resistance genes in bacteria that cause human infections.
How is your work relevant to antimicrobial resistance?
Professor Shiranee Sriskandan: From a clinical perspective, I encounter antimicrobial resistance daily when treating patients. In recent years, we’ve seen an increase in almost-untreatable infections, and the burden of AMR is particularly high in London. We think this is related to the mix of communities amplified by socioeconomic factors and ill health. Although, in the UK, newer antibiotics can be found to manage these cases, this isn’t the case in some parts of the world. My work also involves vaccine and diagnostic development – important tools in tackling AMR, even though the obvious answer might seem to be developing new antibiotics.
"AMR is complex, much like climate change – it requires a multifaceted approach." Dr Andrew Edwards
Dr Andrew Edwards: AMR is complex, much like climate change – it requires a multifaceted approach. My research looks at the molecular mechanisms of resistance, particularly in Gram-negative bacteria, which are at the top of the World Health Organization’s priority list for new treatments. These are a group of bacteria with a special outer layer that makes them harder to kill with antibiotics. These bacteria are particularly concerning because they can quickly acquire resistance to lots of different antibiotics, making infections they cause much harder to treat. So, the work we do is centred around understanding why they're so resistant and then getting to grips with what we can do to overcome that. We’re also exploring ways to improve the efficacy of existing antibiotics by combining them with other agents.
What pathogens are currently the biggest concern in terms of AMR?
Dr Andrew Edwards: Some bacteria are highly resistant but cause relatively few infections, while others, like E. coli, are less resistant but have a high disease burden. This means we use a lot of antibiotics to treat them, which can lead to resistance over time. My work often focuses on E. coli as it’s a good model organism (i.e. it’s easy to work with and representative of several other types of bacteria), and insights here could inform treatments for other pathogens.
"The work that we do in the Centre is very much intertwined with what's happening in healthcare, and we try to synergise with their efforts." Professor Shiranee Sriskandan
Professor Shiranee Sriskandan: In the UK, E. coli is the leading cause of bloodstream infections, with Staphylococcus aureus coming second. Unfortunately, resistant E. coli is relatively common in our local population, so when patients develop a urinary tract infection (UTI) we often find that the infection is resistant to three or four commonly used antibiotics. However, some of the most resistant infections occur in vulnerable patients with other health issues, who have often been exposed to multiple antibiotics; these bacteria might be resistant to an entire list of antibiotics. Preventing the spread of resistant bacteria between patients is critical. It's important to state that the work that we do in the Centre is very much intertwined with what's happening in healthcare, and we try to synergise with their efforts. Preventing transmission is very much tied into our attempts to understand how the bacteria are being transmitted and what makes some bacteria more pathogenic than others.
How can we tackle AMR?
Professor Shiranee Sriskandan: The approach is multi-pronged:
- Prevention – improving diagnostics, infection control, and vaccine development to reduce the need for antibiotics.
- Optimised use – using antibiotics more wisely through better diagnostic tools.
- Treatment development – discovering new antibiotics and alternative treatments, including leveraging the body’s immune system and beneficial bacteria.
"We have to cover our bases and be prepared for whatever mother nature throws at us next." Dr Andrew Edwards
Dr Andrew Edwards: One of the important things to bear in mind is that antibiotic resistance is literally an evolving picture. The organisms that we're most concerned about today might be different from the organisms we're most concerned about in 10 or 15 years’ time. So, the CBRB is not focusing solely on the top two or three organisms. We're looking at quite a broad range of different bacteria that are burdensome, and not just in Western Europe and North America, but also in parts of the world where there are big concerns about multi drug resistant organisms. It’s about trying to understand what's going on today and then trying to understand what might be happening a decade down the line. We have to cover our bases and be prepared for whatever mother nature throws at us next.
What makes the CBRB so special?
Dr Andrew Edwards: Something that we've seen with the centre, but more broadly across Imperial, is a lot more working across faculties. As a centre, we are one of the best examples of long-standing collaboration between the Faculties of Medicine and Life Sciences. That’s been since its inception, 25 years ago, and I think that’s something to celebrate. We're increasingly collaborating with colleagues in engineering, chemistry, mathematics and of course, our clinical colleagues as well. We've seen an increase in the number of clinical academics in the centre and that's very much in line with a broadening of our vision. So, although the fundamental research is still very much at the heart of what we do, we're much more geared towards developing and translating that fundamental knowledge into real world solutions.
Professor Shiranee Sriskandan: I think the unique aspect is our interaction with the clinic. We make sure that the scientific questions we’re addressing are clinically relevant.
Dr Andrew Edwards: I agree. We bring together a very large and unique grouping of scientists and clinicians who are focused on tackling bacterial infection biology. We also work across scales – from molecular interactions to population-level health. For example, we have people who study at the molecular level how proteins interact to cause disease, through to people who have characterised outbreaks of infectious disease and the implications of that for diagnostics and antibiotic usage. A big part of the CBRB’s success is that it is part of the wider infectious disease ecosystem at Imperial. If we look at just AMR, there are more than 100 groups across the university working on this. So, anytime you have an idea, there will be someone you can go and talk to about it, and a way to develop that idea. So, although I think we are a fantastic centre, we also benefit enormously from those around us.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Meesha Patel
Faculty of Medicine Centre
Lou Lee
Faculty of Medicine Centre