Blood protein profiles provide new insights into large-vessel vasculitis
by Meesha Patel
Researchers found that blood profiles of two vasculitis diseases are similar, indicating an overlap in the biology of these diseases.
Scientists have found that two diseases which commonly cause large vessel vasculitis (LVV) have similar blood protein profiles and could be more closely related than previously thought.
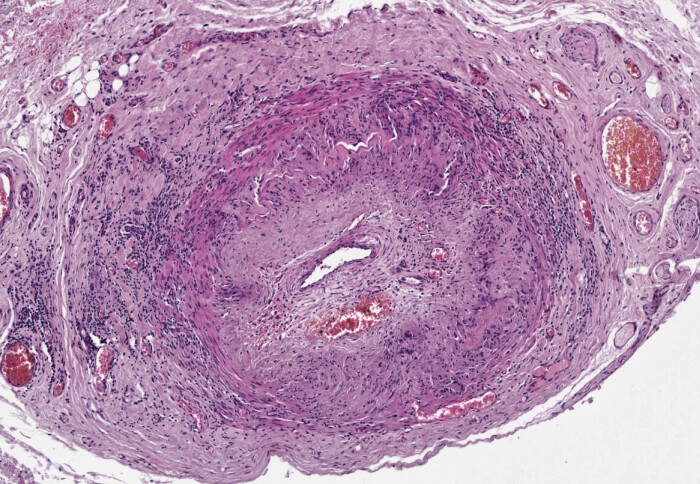
Large vessel vasculitis (LVV) is a condition where branches of blood vessels that carry blood away from the heart are inflamed. It can lead to serious complications like blood vessel narrowing, blockage, sight loss, aneurysm or stroke.
The study published in Arthritis and Rheumatology investigated the blood protein profiles of giant cell giant cell arteritis (GCA) and Takayasu arteritis (TAK), which are traditionally classified as separate diseases because of the age difference in patients and the location of blood vessels. These new findings which suggest an overlap in the biology of these two conditions, are consistent with the view of other experts that these two conditions may be variations of the same disease.
"Our work identifies a protein communication network that is likely to be involved in this process and we believe that the targeted manipulation of such networks would be an effective treatment strategy." Dr Robert Maughan Department of Immunology and Inflammation
The researchers also discovered that both GCA and TAK rely on communication between key immune cells called macrophages, and structural cells in blood vessels which leads to the progression of large vessel vasculitis. The findings have important implications for the care of patients with these diseases, as well as could pave the way for trials which test new treatments.
The study's lead author Dr Robert Maughan from the Department of Immunology and Inflammation said that deeper investigation of the communication between these cells could be an avenue for therapeutics:
“The most severe damage to tissues is often caused by the body’s response to persistent inflammation. In LVV, the response of structural cells in the artery leads to the affected vessels becoming stiff and narrow. Our work identifies a protein communication network that is likely to be involved in this process and we believe that the targeted manipulation of such networks would be an effective treatment strategy. Of course, further research will be required to develop this concept.”
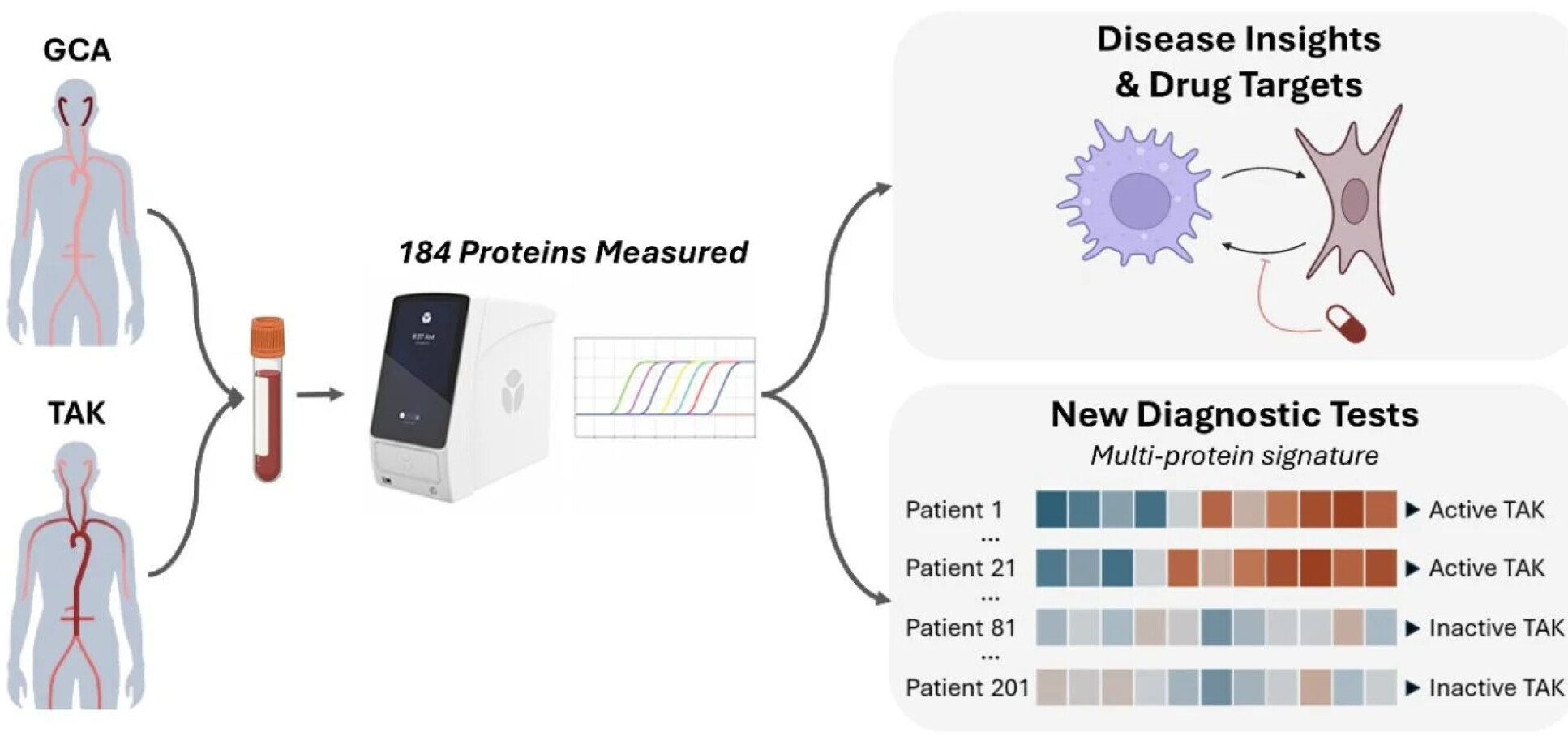
Proteomic blood profiling
Researchers from Imperial College London, University of Leeds and the University of Oxford used a technology called ‘proteomic’ blood profiling which measures the levels of proteins in the blood of nearly 300 patients with GCA or TAK, and unaffected individuals.
"With advances in technology, it is now easier to measure multiple proteins in the blood simultaneously, which is helpful for research and for the development of better blood tests." Dr Robert Maughan, Department of Immunology and Inflammation
Proteins play a critical role in most biological functions, and proteomics can provide a powerful snapshot or profile of a person’s or group’s biological state.
Developing blood tests for large vessel vasculitis
The team’s study also investigated how to develop better blood tests for diagnosing and monitoring LVV diseases.
People with GCA and TAK need regular blood testing to track the progression of their blood vessel damage. However, the current blood tests are not accurate. By harnessing proteomic data, the team could look at blood proteins to create a multi-protein blood test signatures which would be more accurate compared to current tests.
The first author of the paper, Dr Robert Maughan from the Department of Immunology and Inflammation at Imperial College, noted, “With advances in technology, it is now easier to measure multiple proteins in the blood simultaneously, which is helpful for research and for the development of better blood tests. In this study, we found that multi-protein signatures consistently performed better than single-protein tests. More accurate blood tests have the potential to benefit both patients and hospital services by speeding up diagnosis and by reducing the number of other examinations required.”
This study was initiated through an MRC TARGET Partnerships award leading to an ongoing collaborations between the Imperial, Leeds and Oxford NIHR Biomedical Research Centres with additional funding from NIHR, Vasculities UK, the Medical Research Foundation and UKRI.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Meesha Patel
Faculty of Medicine Centre