Addressing molecular-level barriers to brain tumour treatment
Brain artwork in the Main Entrance of Imperial College London
Delivering drug treatments to the brain is a challenge requiring multidisciplinary understanding of the blood brain barrier, brain tissue and drugs
The Institute for Molecular Science and Engineering (IMSE) brought together a team from experts at Imperial to provide a state of the art of drug delivery to the brain and recommend policy changes that could improve both technology development and ultimately patient treatment. Authors include researchers with expertise on drug transport, interfaces between materials and cells, neuroscientists, experts on surgical interventions, neurosurgeons, oncologists, and those with knowledge on computational modelling to streamline drug development.
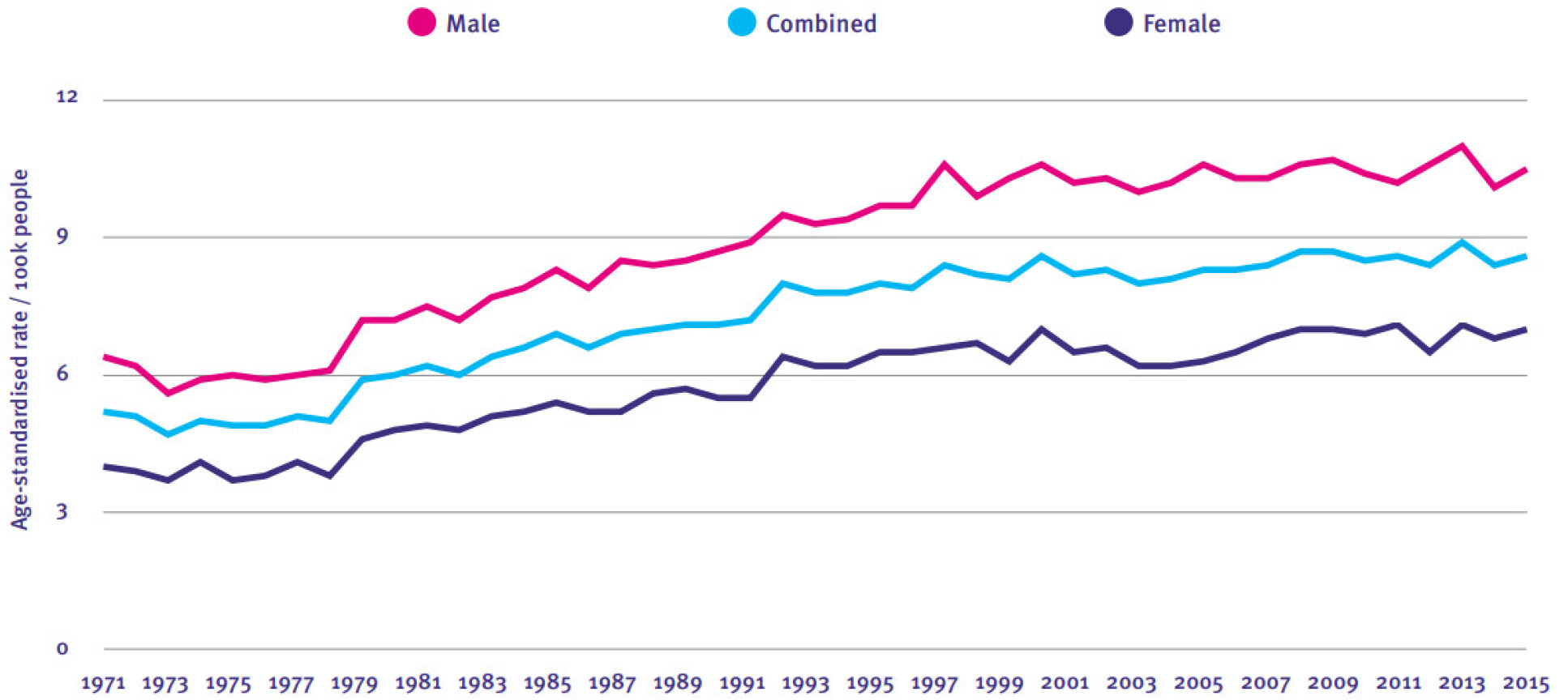
Brain cancers are some of the most lethal brain diseases. The latest briefing paper published by IMSE explains the complexity of delivering drug treatments to the brain with a focus on glioblastoma (GBM). The number of new GBM cases per year in England is ~5 per 100,000 people and the survival rates are low; only 25% of patients survive two years after diagnosis, even with aggressive treatment.
A key difficulty in treating these tumours is delivering the medication to the brain through the blood brain barrier (BBB). The BBB is formed by tightly connected endothelial cells that regulate the movement of ions, molecules and cells between blood and the central nervous system. Only small molecules can passively diffuse through the BBB, meaning 95% of drugs cannot reach brain tumours. Moreover, glioblastoma damages the BBB junctions, complicating the distribution of drugs into the affected areas of the brain in an homogenous manner.
Because of this, researchers are developing new methods to either traverse through or bypass the BBB. These techniques sometimes involve modifying the drug at the molecular level. This briefing paper summarises the latest advances in treating GBM, including the development of delivery agents such as nanocarriers, microbubbles and even bacteriophages, non-pathogenic viruses with a natural ability to cross the BBB. A comprehensive comparison between these methods is presented in the briefing, including the state of development of the treatments, either at early R&D or approaching clinical trials.

This paper also considers the molecular environment of the central nervous system. It is important to understand how the brain tissue will interact with the drug once the latter has gone through the BBB to design effective treatments. The density and stiffness of brain tissues change in glioblastoma which could lead to an additional barrier or dilution of the drug.
Authors also highlight the importance of imaging techniques to first characterise the tissue, and then track the effectiveness of treatments. All of these variables mean that new advances in the GBM treatment field require interdisciplinary teams, comprising molecular-level understanding of biochemistry, biomechanics, medical robotics, advanced computational models and clinical expertise.
The paper calls for long-term strategic investment in neuroscience to build a strong research community and develop networks that can deliver breakthroughs. Authors also encourage multidisciplinary approaches bringing together basic science and clinical researchers, computational and translational communities. Developing a pool of multidisciplinary experts through postgraduate training as well as clinical fellowships will be key to achieving this approach. Importantly, research should extend into the NHS, a national asset that can provide access to patients. The paper urges investment to extend the capacity to deliver clinical trials and more support for national brain tissue banks, as well as regulation of these trials with international standards to maximise participation. And they finish by bringing the attention to translation to ensure that advances will reach the clinical setting and therefore those affected by brain cancers.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Elena Corujo Simon
Faculty of Engineering