 In her role as Head of Undergraduate Primary Care Teaching at Imperial, Dr Sonia Kumar is helping to prepare medical students to face the challenge of working as a qualified doctor. They will join the NHS at a time when it is having to cope with the health consequences of people living longer, while simultaneously facing ever squeezed budgets. Arguably there could not be a more challenging time to join the profession and Dr Kumar says students often feel ill-prepared for the job ahead of them.
In her role as Head of Undergraduate Primary Care Teaching at Imperial, Dr Sonia Kumar is helping to prepare medical students to face the challenge of working as a qualified doctor. They will join the NHS at a time when it is having to cope with the health consequences of people living longer, while simultaneously facing ever squeezed budgets. Arguably there could not be a more challenging time to join the profession and Dr Kumar says students often feel ill-prepared for the job ahead of them.
She explains: “One problem with medical education is that it’s taught in blocks – students study one area at a time, they are tested on it, then they move on to something else. But treating patients couldn’t be more different – you might be working with a pregnant woman who also had MS, who also has a child with asthma.”
Student comment
“Everything I have learnt on this placement, I could not have learnt from a book or online resource. It was all about meeting patients and healthcare professionals in their environment and absorbing the content of interactions and patients' narratives. It is an attachment that definitely stands out as memorable throughout the whole six years of medical school.”
An alternative, already gaining traction in medical education in the US is known as the longitudinal clerkship. It is based around a more holistic approach to medicine where students spend more time with individual patients learning about their conditions, their needs and how they can be helped.
This approach is now being trialled by a group of 24 students at Imperial. For one year, they spend a day a week in General Practice with a case load of patients. For example, a student might work with a pregnant woman, attending antenatal appointments and ultrasound scans, then continuing to visit her following birth and as her baby grows.
Dr Kumar says the authenticity of the experience fundamentally changes the students identities: “We are already gathering evidence that this approach leads to better learning and a more meaningful experience for the students. Those who are taking part see themselves differently – not as medical students but as student doctors.”
“There are benefits for the patient too – they gain an advocate and someone who can take the time to help them better understand what has happened in the often very short interaction they’ve had with their doctor.”
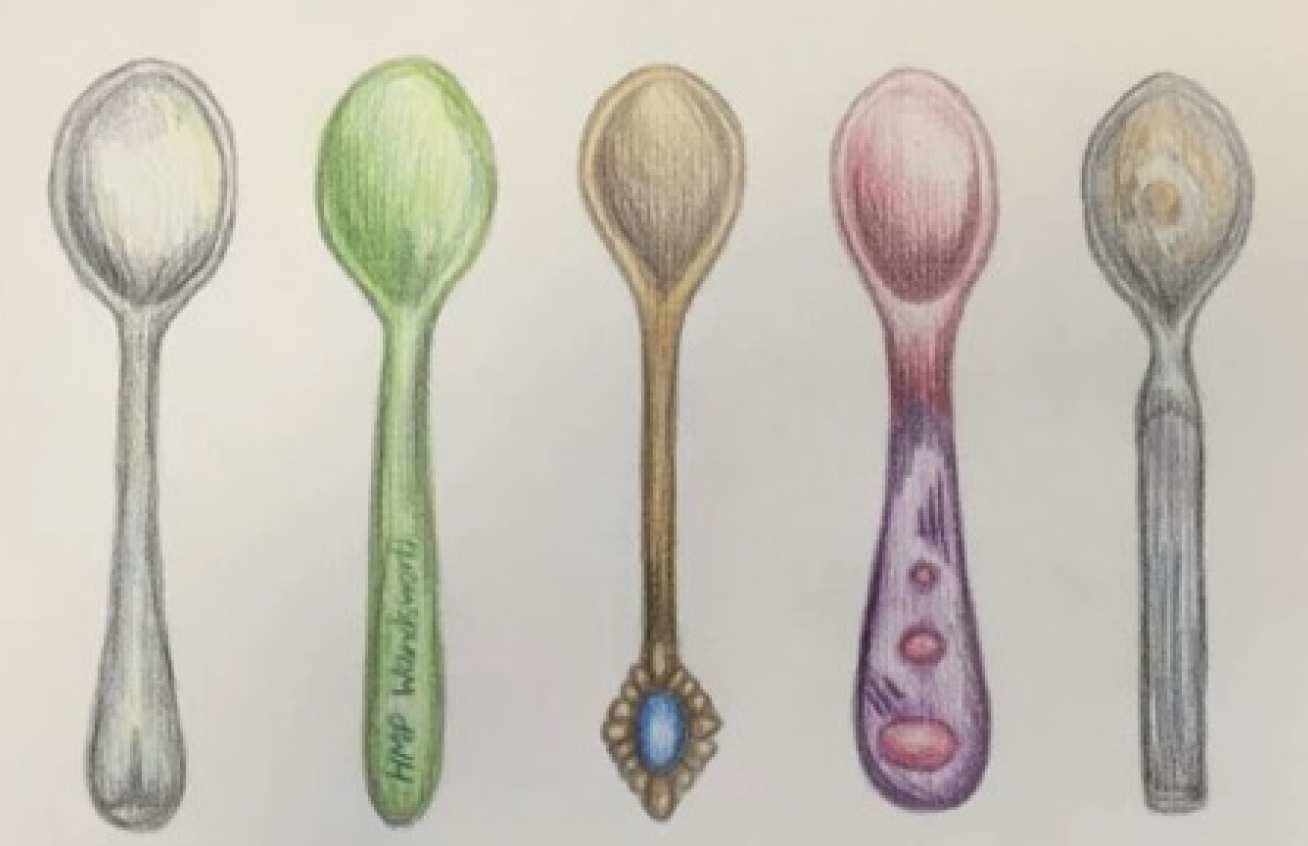
Alongside their traditional academic outputs, students are asked to produce a creative piece of work, which could be writing, music, art or photography, to reflect on their experiences. This encourages students to think about their own values and boosts their empathy for patients. This creative assessment approach has also been used with powerful results, in an optional module developed for students in their final year (see below).
The longitudinal clerkship model has proved successful and now Dr Kumar’s team have developed a second pilot - a ten-week general practice attachment for third year students. This has included a number of innovative sessions with a wide variety of people, conditions and settings, from patients in prison to a cancer patient receiving palliative care.
Trying a new formula
Dr Kumar clearly values the use of evidence in medical education and has worked with Imperial’s Educational Development Unit (EDU) to help push forward best practice. She says: “We have an open dialogue with staff at the EDU and that’s important. We need education research to demonstrate impact, and we need to share what we’ve learnt.”
By collaborating with the EDU and with colleagues within the medical school, Dr Kumar’s team now has 13 innovative placements up and running, ranging from studying dermatology using art and sculpture, to learning about health inequalities by working at a food bank or refugee clinic.
Reflecting on what she and her team have achieved so far, Dr Kumar said: “I think you have to look for opportunities and, sometimes, create your own ones. It’s difficult, but I believe that you can’t let the day-to-day get in the way of your long-term plans and vision.”
Sign Up
If you are interested in receiving the Learning and Teaching Newsletter, please email ltstrategy@ic.ac.uk.
You can also view the issue archive online.

